Celebrating the global shift in women’s health - and an opportunity to improve health for women with MS around menopause
NewsThis article has been collaboratively written by postgraduate researcher Suzanne Britt, neurologist Dr Kate Petheram and MS specialist nurse Ruth Stross, with support from health writer Charlie Peel. Ruth is also our head of nursing for Neurology Academy.
MS is nearly three times more common in women than in men. The median age of females with a new diagnosis of MS is 40 to 44 years. In total 93% of new female cases are of working age (under 65 years of age).
Menopause typically occurs in women between the ages of 45 and 55 years, so in MS 30% of the population are peri or postmenopausal women. In the Women’s Health Strategy public survey only 9% of respondents said they have enough information about the menopause and less than 64% felt comfortable talking to healthcare professionals about it. (Brown 2024)
“The menopause transition often coincides with substantial midlife stresses, health conditions, and role transitions, which increase individuals’ vulnerability to depression.”
Brown et al, Lancet, 2024
Many respondents reported finding it difficult to access appropriate menopause care. This was reported as being due to a lack of recognition of symptoms from both women and healthcare professionals, with some written submissions noting that symptoms of the menopause can be confused with other conditions, such as women sometimes being prescribed antidepressants rather than menopause treatments.
We now recognise that there is significant overlap in symptoms between those of MS and perimenopause or menopause (figure 1). These symptoms include urinary and sexual dysfunction, memory disturbance, mood changes and fatigue, among others and can also affect physical, emotional, mental and social wellbeing (Giovannoni et al 2024). Healthcare professionals may not be aware of this overlap which leads to delays in symptoms being treated appropriately (figure 2). This also leads to frustration for women who may not know where to turn to for advice.
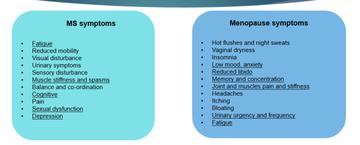
Figure 1: The overlap of MS and menopausal symptoms
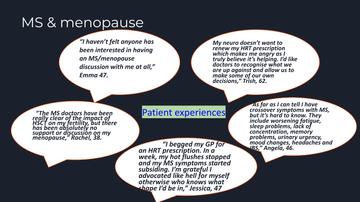
Figure 2: Comments from women with MS about their menopause experience (shared with thanks from work by Rachel Horne)
The Woman's Health Strategy for England (August 2022) recognises that whilst women live longer than men they spend longer in poor health. It also notes that, historically, the healthcare system has been set up by, and for, men. The ambition set out in the paper is to boost health outcomes for women and girls with a 10 year plan. It acknowledges that lots of work has been done already and lays out priority areas and plans for change. Menopause is identified as a priority area and one of the key themes is information and education. Neurologists are specifically highlighted as a group of healthcare professionals who need to have a basic understanding of menopause and to signpost women to appropriate support (figure 3).

Figure 3. Quote from the Women's Health Strategy 2022
There is a need for this to change. Ideally, there needs to be a growing awareness of how the intersecting experiences of women’s lives affect how they access support for their MS at pivotal points in their lives. Conversations about issues pertaining to age, ethnicity, class, education, economic status,and mental health can shape the way that women with MS meet and experience services and are needed within health, the workplace and our wider society. Figure 4 shows some of the multiple factors shaping individual experiences of healthcare and indicates how services might support these (left) or further exacerbate their negative effects (right).
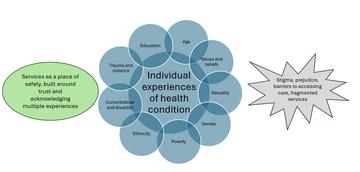
Figure 4: Infograph created by Suzanne Britt demonstrating the intersecting factors influencing individual experiences of a health condition.
All women, as well as GPs, neurologists, MS nurses and other healthcare professionals working with them, need to be armed with the information they need to enable women with MS who are going through the menopause to have open discussions around their MS and menopause symptoms (Glinkos, Dobson 2023).
Access to holistic and symptom-based care that wraps around their individual needs at a time when their health and psychosocial needs are evolving will support their self-management of MS and menopause. Peri and menopause are a normal part of ageing for half of our global population. The process takes around 10-15 years, and women live postmenopausally for around a third of their lives; the importance of managing it well for optimal quality of life during and post menopause cannot be overstated (Lancet series 2024).
Shared decision-making and using up-to-date patient pathways such as the Optimum clinical pathway for MS are key to ensuring optimal patient care (figure 5), and can have a positive impact on quality of life for the individual (Lorefice et al 2023). Women and healthcare professionals need access to the most current information to make informed choices about treatments such as hormone-replacement therapy (HRT) in a personalised way.
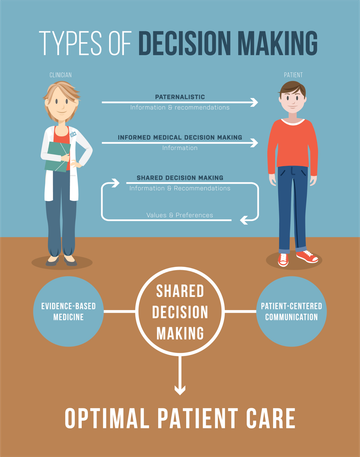
Figure 5: decision-making for optimal patient care
It is important that GPs are aware that living with MS or being on a disease-modifying treatment (DMT) is not a contraindication for HRT, and that the variety of HRT options available can be tailored to fit needs and preferences alike. Likewise it is imperative that neurologists consider whether the symptoms a woman is presenting with are related to her MS or her hormonal changes. This should then be factored into appropriate treatment and management plans, with referrals to relevant healthcare professionals and signposting to information and support to empower self-management.
Underpinning all of this is the need for appropriate lifestyle advice during perimenopause and menopause. An explanation of the stages of menopause needs to be shared with women, along with the benefits and risks of lifestyle management and therapeutic options for menopausal symptoms to complement any potential medication changes. Some strategies have been suggested for managing MS and menopause related symptoms concomitantly (Giovannoni et al 2024) (figure 6).
There is so much energy and action around menopause including the menopause workplace pledge led by the Wellbeing of Women charity, the Midlife MOT, the updated NICE guidance for menopause and the menopause workplace toolkit (Dec 2023). This is an opportune moment to use this energy and momentum to shed a light on the experiences of women living with MS during menopause - and to capitalise on the opportunities to improve those experiences for the duration of their years in the menopausal transition.

Figure 6: Table taken from 'MS care: integrating advanced therapies and holistic management', Giovannoni et al 2024
The Woman's Health Strategy for England's 10-year ambitions are:
Everyone – girls and boys – is well informed about menopause from an early age. Awareness across the whole population of the menopause is increased and the menopause is no longer a taboo subject in any part of society
Women going through the perimenopause and menopause can recognise symptoms and know their options, including self-care and where to seek support
Women can access high-quality, personalised menopause care within primary care and, if needed, specialist care in a timely manner, and disparities in access to menopause treatment are reduced. Women are able to access the full range of treatment options, including contraception for the management of menopause symptoms. All menopausal women for whom HRT is suitable are able to access HRT and at a reduced cost
Women and girls experiencing early menopause – whether naturally or as a side effect of medical treatment – can access specialist and personalised support, including support for mental health, fertility and bone health
Healthcare professionals in primary care are well informed about the menopause, and able to offer women evidence-based advice and treatment options, including HRT and alternatives
Other healthcare professionals – for example cardiologists or neurologists – have a basic understanding of menopause, including awareness of symptoms and future health risks associated with menopause, and can signpost women to appropriate support
Women are supported to remain in the workplace and employers are well equipped to support their workforce during the menopause. Employers are encouraged to implement evidence-based workplace support for the menopause, including introducing workplace menopause policies
There is increased research into the menopause, including different treatment options and impacts of menopause or menopause treatment on future health risks
Related articles
Encouraging excellence, developing leaders, inspiring change
MS Academy was established in 2016 and in that time has accomplished a huge amount with exciting feedback demonstrating delegates feel inspired and energised along their personal and service development journeys. The various different levels of specialist MS training we offer are dedicated to case-based learning and practical application of cutting edge research.


