An audit of outpatient consultation for patients with chronic multiple sclerosis
In common with many district general hospitals, there are no specialist MS clinics at St Richard’s, Western Sussex Hospitals NHS Trust. Patients with MS are seen in the general neurology clinics alongside those otherwise neurologically afflicted. Such a run of the mill approach predisposes the clinician to a poorly structured consultation. It can be difficult to approach the MS patient in the right gear if he is sandwiched between a newly diagnosed motor neurone disease patient and one with functional neurological illness. The content of consultations with the chronic MS sufferers tends to be patient led. The 15 to 20 minute clinic slot is easily filled, the doctor responding to whatever the most pressing need is from the patient’s point of view at that time. Alternatively, the consultation may be completely dominated by the patient responding to the topic most interesting to the doctor, often the disease-modifying drug, and attention diverted away from important, but less diverting concerns.
NICE Guidance for the Management of Multiple Sclerosis in Adults (2014) recommends a more proactive and systematic approach. Obviously the patient’s wishes must be addressed, but this should be as part of a thoroughly comprehensive consultation process. A review of their disease, general health, social activity and participation, their care and carers, a medication review, a bone health review, a review of particular concerns regarding those with severely reduced mobility and referral to allied services, should all be taken into account according to that considered appropriate to each individual’s care.
The guidance states that we should “ensure that all people with MS have a comprehensive review of all aspects of their care at least once a year,” and that “the comprehensive review is carried out by healthcare professionals with expertise in MS and its complications.” Standards are then set down for each aspect of the clinician’s enquiry. Described below, our audit set out to determine how well our clinic consultations adhered to the NICE standards.
Audit method
Number of medical notes audited: 52
Sampling method: Notes were sampled from the MS alerts register on Sema Helix, our hospital patient administration system. At the time of auditing, there were 475 patients with MS alerts for St Richard’s. Notes were requested in alphabetical sequence by the neurology secretaries. In total, 70 sets were ordered and of those 52 were available for the audit.
Standards used: The audit was based on the NICE Guidance for the Management of Multiple Sclerosis in Adults 2014, in accordance with a set of standards proposed for when patients attend for “a comprehensive review of all aspects of their care at least once a year”.
Material audited: All written documentation made by MS clinicians at St Richard’s between 01/01/16 to 31/12/16 was used for the audit. This involved the records made by three neurologists, one neurorehabilitation consultant and one MS nurse specialist. Written documentation included hand written notes taken at the time of the consultation and clinic letters.
Audit period: An audit period of 12 months from 01/01/16 to 31/12/16 was used.
Exclusion criteria: A pragmatic approach was adopted so that only the notes which were immediately available from medical records were audited.
There were some patients who were included in the audit for the purposes of collecting baseline data, but who did not go on to have their notes audited. There were:
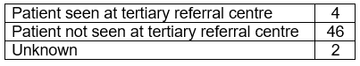
- Patients who had been reviewed at a tertiary referral centre during the audit period. They may have been assumed to have had a comprehensive review at the tertiary centre which was therefore not duplicated at St Richard’s. The aim was to audit the practice of our clinicians and not that of those outside the trust.
- Patients who had not been seen by an MS clinician within the audit period
Auditors: All five MS clinicians were involved in the auditing process.
Audit results
Baseline data
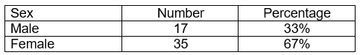
Patient sex
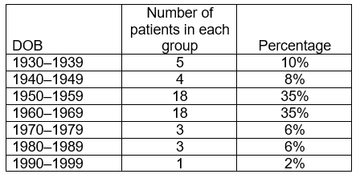
Patient date of birth
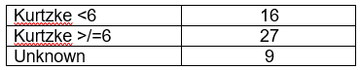
Kurtzke score > or =6
(K=6 equates to requiring a walking aid to walk 100m)
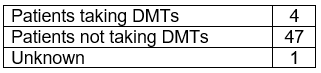
Taking disease modifying treatments during the audit period
Seen at tertiary referral centre during the audit period
Audit standards
1.6.1 Is there written evidence to show that the patient been seen as an outpatient at St Richard’s or in the community on at least one occasion by a health care professional with expertise in MS within the audit period? i.e. a neurology or neurorehab doctor at St Richard’s or an MS nurse specialist?
In all cases, written evidence was documented in the medical notes where there had been contact with an MS clinician.
Patient notes were only included in the auditing process from this point on:
- If the patient had had contact with an MS clinician within the audit period
- If the patient had not been seen at a tertiary referral centre within the audit period
27 patients met these criteria
1.6.3 Has there been a comprehensive review of MS symptoms as follows?
Has there been enquiry about visual disturbance?
Yes, 6
No, 21Has there been enquiry about speech and swallowing?
Yes, 8
No, 19Has there been enquiry about recurrent chest infections?
Yes, 9
No, 18
We noted that this enquiry was made for all patients where there had been an enquiry about speech and swallowing.
Has there been enquiry about upper limb function (weakness, sensory disturbance, tremor, ataxia, spasms, spasticity?)
Yes, 13
No, 14Has there been enquiry about urinary symptoms, including catheter issues?
Yes, 21
No, 6Has there been enquiry about urinary tract infections?
Yes, 17
No, 10
We noted that this of the 21 patients where an enquiry had been made about urinary symptoms, 17 had been asked about UTIs.
Has there been enquiry about bowels?
Yes, 14
No, 12
Not answered, 1Has there been enquiry about sexual function?
Yes, 0
No, 27Has there been enquiry about lower limb function (weakness, sensory disturbance, tremor, ataxia, spasms, spasticity?)
Yes, 22
No, 5Has there been enquiry about mobility?
Yes, 18
No, 9
We noted that this of the 22 patients in whom an enquiry was made about lower limb function, 17 were asked about mobility. Of the five patients in whom no enquiry was made about lower limb function, only one was asked about mobility.
Has there been enquiry about balance and falls?
Yes, 10
No, 16
N/A, 1Has there been enquiry about pain?
Yes, 14
No, 13Has there been enquiry about fatigue?
Yes, 7
No, 20Has there been enquiry about depression?
Yes, 7
No, 19
Not answered, 1Has there been enquiry about cognitive disturbance?
Yes, 4
No, 22
Not answered, 1Has there been an enquiry about sleep disturbance?
Yes, 3
No, 23
Not answered, 11.6.3 Is there documentation regarding MS disease course? ie documentation of relapses, or of progression of existing problems
Yes, 14
No, 11
Not answered, 21.6.3 Has there been a review of the patient’s general health? Examples: cannabis use, exercise,
Yes, 3
No, 12
Not answered, 12Has there been enquiry about weight?
Yes, 10
No, 17Has there been enquiry about smoking?
Yes, 2
No, 25Has there been enquiry about alcohol use?
Yes, 1
No, 26Has there been enquiry about contraception use?
Yes, 0
No, 18
N/A, 9Has there been enquiry about the patient’s other medical conditions, including access to routine health screening?
Yes, 5
No, 20
Not answered, 21.6.3 Has there been an enquiry about social history? Especially social circumstances, employment, daily activities, leisure activities, driving and access to transport
Yes, 10
No, 171.6.3 Has there been enquiry about personal and social care needs and disability aids?
Yes, 10
No, 171.6.4
Has a referral been made to any members of the MS team?
Yes, 14
No, 131.6.5 Has there been a medication review as follows: Is the current medication documented?
Yes, 15
No, 12Is the patient taking vitamin D supplements?
Yes, 6
No, 21Is there evidence of a medication review?
Yes, 14
No, 131.6.6 Has there been a bone health review? (Poor mobility, low BMI, smoking and alcohol all influence bone health)
Yes, 3
No, 241.6.7 If severely reduced mobility, is a system in place to ensure that the patient is regularly assessed and reviewed for risk of contractures and pressure ulcers?
Yes, 4
No, 12
N/A, 111.6.8 If severely reduced mobility, has the patient been checked for contractures and areas at risk of pressure ulcers at every appointment?
Yes, 6
No, 11
N/A, 101.6.9 Has an enquiry been made about care provided by carers?
Yes, 3
No, 18
N/A, 61.6.9 Has the carer been made aware of their right to a local authority carer’s assessment?
Yes, 0
No, 20
N/A, 71.6.10 Has the patient been referred to palliative care services for end of life care if appropriate?
Yes, 0
No, 8
N/A, 19
What happened to the 23 patients who were not reviewed during the audit period?
There was no written evidence in our hospital records for 23 (44%) of the audit cohort having been reviewed for their MS during the audit period.
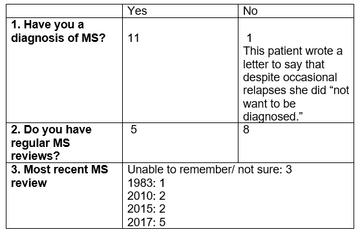
In November 2017 questionnaires were posted to all 23 patients. They were asked the following questions:
- As far as you are aware, do you have a diagnosis of MS?
- Specifically for the management of your MS, do you have regular reviews (at least once a year) of the problems associated with your MS? This might be by a neurologist, neurorehabilitation doctor, GP or multiple sclerosis nurse.
- When was the last time you had an appointment for review of your multiple sclerosis?
A month later, 12 replies have been received., with responses as follows:
Discussion
Our task was to determine how well our outpatient clinic practice matched the standard of care set out in the NICE Guidance for the Management of Multiple Sclerosis in Adults 2014. This recommends that patients with MS are given a ‘comprehensive review of all aspects of their care at least once a year” (Section 1.6)
Fifty-two consecutive sets of available patient notes for our hospital were retrieved according to our MS register. All written documentation made by MS clinicians (i.e. St Richard’s neurologists, the neurorehabilitation physician and the MS nurse specialist,) between 01/01/16 and 31/12/16 was audited. At least 27 (52%) of the 52 patients had a Kurtzke score of greater than or equal to 6 (patient requires a walking aid to walk 100m.) However, in nine cases, the Kurtzke score was unknown, having either not been explicitly recorded or being unable to be inferred from the medical notes.
Twenty-three patients (44%) had no written evidence of having been seen during the audit period. Their notes could therefore not be used to measure our performance against the NICE standards. A further two patients had been seen at tertiary referral centres during the audit period and these were also excluded from analysis; any appraisal made at the tertiary centre may not have been done at St Richard’s to avoid duplication of effort. This left 27 patients whose notes were suitable for the standards’ analysis.
For almost every standard recommended, there was evidence of an enquiry being made in fewer than 50% of the patients. In many areas enquiries were made of 25% or fewer patients. This included enquiries about visual disturbance, sexual function, fatigue, depression, cognitive disturbance, sleep disturbance, general health, smoking, alcohol use, contraception, comorbidities, vitamin D supplements, bone health, and carer involvement. For many of these issues pharmacological or other solutions are readily available and opportunities were lost to offer help which might have been of significant benefit to the patient.
In only 25% of patients in whom it would have been appropriate, was there any documentation of a system in place to regularly assess for pressure ulcers and contractures although just over half of these had been checked for pressure ulcers and contractures at the time of their review.
In some domains our performance was better. Those in which 50% or more enquiries were made include enquiries about upper limb function, urinary symptoms and urinary tract infections, bowel issues, lower limb function, mobility, pain, disease course. Additionally in 50% or more, a referral had been made to other members of the MS team, and there had been a documented medication review.
It is more difficult to determine how well we complied with guidance to refer to palliative care services. It is difficult to judge from the patient record whether or not such a referral would have been beneficial. However, none of the patients in our audit were referred.
Of concern are the 23 patients in whom there was no documentary evidence of an MS review during the audit period. Twelve of these responded to a postal enquiry sent out in November 2017. All 12 either had a diagnosis of MS or probably had a diagnosis of MS (one patient also responded with a letter to say that she dis not want to know whether she had the disease or not, but her symptom account made the diagnosis very likely). Of these five had had their MS reviewed in 2017, and eight had either not had any review since 2010 or could not remember when the most recent review had taken place.
Assuming that this sample is typical of the 475 patients with MS on our register, and that the documentary evidence is a reasonable proxy for the substantive content of the consultation itself, two major problems with our review system are immediately apparent: Firstly, that almost half of our patients with MS are not getting an annual review, and that some are not under any review at all. Evidence as to why this should be is incomplete, but those who responded to our subsequent investigation were living within our catchment area and had an established diagnosis of MS. They were therefore manifestly appropriate for an annual review by one of our clinicians. Secondly, for those who did get reviewed during the audit period, the process was not at all a comprehensive one. In some cases, patients had been seen more than once during the audit period. Even then, taking the documentary evidence of all the consultations as a whole, the enquiries were made in a patchy way, concentrating on only a few issues.
Once again, I am indebted to the Neurology Academy for their ongoing encouragement and support. The challenge we face now is to try and find a solution. It must be one that facilitates the process of a comprehensive patient review in line with the NICE Guidance, is helpful to the consultation process without being burdensome, and does not overwhelm already over-stretched clinicians.
Should there be other Academy experts who have any helpful suggestions as to how this might be done, we would welcome your advice. Please get in touch via The Academy.
More MS Academy Service audit Projects
Encouraging excellence, developing leaders, inspiring change
MS Academy was established in 2016 and in that time has accomplished a huge amount with exciting feedback demonstrating delegates feel inspired and energised along their personal and service development journeys. The various different levels of specialist MS training we offer are dedicated to case-based learning and practical application of cutting edge research.