Before you watch this webinar
Enhancing your learning experience begins with understanding you better. Collecting data enables us to tailor our educational content specifically for our audience. Discover more about how we handle your information in our Privacy Policy.
Event
The use of biomarkers and CSF analysis in patients with MS and neurological presentations during the COVID-19 pandemic
Presentation slides
Summary
This summary covers:
- COVID-19 movement into the brain
- Central nervous system
- Parallels to SARS-CoV
- How do we examine CSF for COVID-19?
- Research and healthcare logistics during a pandemic
The session looked at biomarkers that have been tested for and will review what is understood about the pathophysiology of the disease.
Sharmilee briefly summarised her key points at the end of her webinar (20.46). She noted that there is a lack of knowledge about the CNS involvement in COVID-19 at present, but it is clear that lymphopaenia may point to a more severe outcome (4.48), also suggesting that there is a direct role for viral injury. It is important that we now try to risk stratify patients, and that we find ways to continue with existing investigative work which has stopped as a result of the pandemic (18.22).
COVID-19 movement into the brain
There have not been any publications for TSS findings in COVID-19 and there have been messages circulating that it doesn’t involve the brain. However, based on evidence gathered in China and Italy it is becoming apparent that this is not the case.
Named COVID-19 because it appeared to the globe in 2019, it is remarkably similar to the COVID strain SARS and appears to move in the same way throughout the body, beginning in the respiratory tract and moving downwards towards the lungs, and upwards, through the nasal tract, to the brain (fig 1).
Figure 1: Diagram demonstrating how the COVID-19 virus is thought to move through the body.MS
Central nervous system
There is uncertainty as to how much of the central nervous system is affected at the outset (3.06). People anecdotally experience dizziness and cognitive fog as with influenza. More recent deaths attributed to respiratory failure may possibly be linked to brainstem involvement.
Sharmilee looked at a number of pre-peer review research papers (3.21) looking at neurological presentations. Evidence from Wuhan looking at 216 cases found that 36.4% had some level of neurological involvement, whilst a review in JAMA looking at hypertension as a risk factor for mortality also highlighted a central nervous system component.
There is evidence that, in those with more severe disease, lymphopaenia is a particular problem (4.48) as a comorbid element as is a rise in urea. Highlighting the subpopulations in the lymphocytes of COVID-19 infected patients as compared to non-COVID-19 patients with pneumonia (fig 2), Sharmilee noted that the numbers behave in a way that would indicate a virus directly interacting with the lymphocytes – something that occurs in viruses that sabotage the immune system by overwhelming it. This can be seen in the non-severe disease patients as well, suggesting a compromised immune system in all COVID-19 patients.
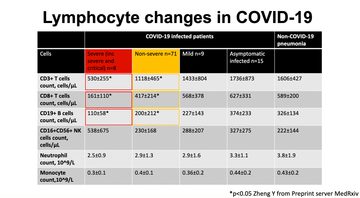
Figure 2: Lymphocyte changes in COVID-19 as sourced from Zheng Y, via Preprint server MedRxiv
Sharmilee suggests that this data calls into question whether the virus affects a cytokine store and causes the lung problems in patients – whether it is an overactivity of the immune system – or an immune system which is compromised by the virus. There is an impression given by the data that the virus is directly attacking the immune system (8.52).
Parallels to SARS-CoV
We know that the receptor site which the virus attaches to is the same for both the SARS-CoV and the current COVID-19. However, SARS-CoV is understood to be a respiratory distress syndrome (9.56) which enters the body via the olfactory bulb and has a rapid transneuronal spread to areas in the brain. In SARS, where death results, it is usually from dysfunction or death of infected neurones, especially those found in the cardio-respiratory centres in the medulla.
To date, COVID-19 has appeared to be pulmonary failure rather than something happening in the brain. As yet, there has been no evidence gathered from CSF analysis or autopsy data for COVID-19 in the brain, although there are studies underway including one in Italy (12.08).
How do we examine CSF for COVID-19?
Sharmilee explained that the best approach to testing whether COVID-19 affects the brain is to test for all known inflammatory mediated neuronal damage biomarkers, all of which are well-validated and studied and these were discussed in detail (12.44).
She then went on to demonstrate the various ways that we can look at this in MS patients in more detail. She displayed an MRI of a female MS patient in her 30’s to demonstrate the neurofilament levels in her brain (14.46), and showed how blood neurofilaments can be used in patient profiling (15.48). She also showed the progression rates of neurofilaments in a patient with ALS (14.40) as an example of how we can look for changes in people with COVID-19.
Research and healthcare logistics during a pandemic
A key challenge of carrying out investigations during a pandemic is the need to prioritise clinical practice (17.36) tied with the need to keep at-risk patients away from hubs or care to avoid the spread of the virus. Sharmilee discussed some of the logistical challenges that she and her team have contended with whilst trying to carry out neurofilament testing in order to better understand COVID-19 (18.22). To minimise risk, using telemedicine to ascertain what tests are needed followed by procedures carried out locally in an out-patient setting. Samples can be couriered in the same day to a central hub for analysis. Sharmillee highlighted that, with a large number of laboratories being set up to carry out PCR tests for COVID-19, there is a higher rate of variability which needs working on. Citing that the sensitivity of PCR gives a 72% accuracy, versus a CT chest examination which has a 98% accuracy, demonstrating room for improvement (19.32).
Were you registered on this course?
Log in to access resources..
LoginEncouraging excellence, developing leaders, inspiring change
MS Academy was established in 2016 and in that time has accomplished a huge amount with exciting feedback demonstrating delegates feel inspired and energised along their personal and service development journeys. The various different levels of specialist MS training we offer are dedicated to case-based learning and practical application of cutting edge research.
