Evaluation of the Extended Pharmacy Service for Neurosciences Wards at KCH on Saturdays
Poster
Introduction
Prior to the extended Saturday service, on a weekday basis the neuropharmacy team reviewed neurosurgery patients pre-operatively in the neuro-admissions lounge (NAL) as well as screening all patients on all five neurosciences wards. This involved undertaking medication reconciliations, prescribing regular medications, prescribing and educating patients on post-operative medication and enabling efficient and safe discharges by processing drug lists.
The neurosurgeons approached the neuropharmacy team requesting an enhanced pharmacy service on Saturdays to help facilitate the increasing number of weekend lists and relieve work pressures on the neurosurgical trainees. A business case was put together and a neurosciences pharmacist position funded to facilitate this enhanced weekend service.
The enhanced pharmacy service was scoped out to be a 7:30-3:30 full working day, which was to include pharmacist review of all patients triaged through the NAL. The enhanced service would also include medication reconciliation for new patients on all other neurosciences wards, prescribing of regular medication, review of ICU step downs and clinical reviews of any high risk patients identified by the week team or staff.
Due to the COVID pandemic this service was never truly implemented and instead a general enhanced pharmacy service has been provided between 8:00 and 12:00 on Saturdays. We have collected data over eight weeks to evaluate the Saturday service to determine the impact of pharmacy presence on the wards to review its efficiency and impact on the workload.
Objective
1. Safely Stepdown ITU patients
a) Measure number of ITU stepdown patients stepped down to neurosciences wards Friday evening/Saturday morning and percentage of which were seen by the pharmacist during the Saturday service.
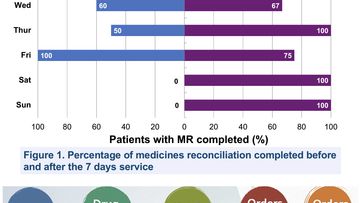
2. Complete Medicines Reconciliation for New Admissions
a) Measure the number new admissions to neurosciences wards on Friday evening/Saturday morning and the percentage of which were seen by the pharmacist during the Saturday service.
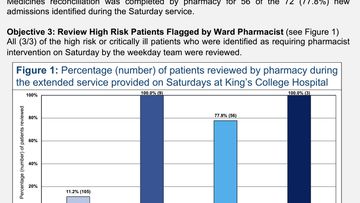
3. Review High Risk Patients Flagged by Ward Pharmacist
a) Measure number of critically ill patients identified for review by the regular pharmacy team/MDT members and the percentage of which were seen by the pharmacist during the Saturday service.
4. Supply Medicines Required
a) Measure number of stock orders processed
b) Measure number of non-stock orders processed
5. Provide Clinical Interventions to Ensure Best Patient Care
a) Measure number of prescribing/de-prescribing interventions made on each ward
b) Measure number of discharge drug lists written by the pharmacist on each ward
c) Measure number of patients/carers educated on each ward
d) Measure number of staff members provided with medicines information on each ward.
e) Measure number of other interventions (e.g. VTE assessments, antibiotic reviews advised, allergies documented) on each ward.
Service development
- The service evaluation took place at the Denmark Hill site over an eight week period between June 2021 and July 2021.
- The evaluation took place on the neurosciences wards: Kinnier Wilson Ward & HDU, Murray Falconer, David Marsden and Charles Polkey.
- The data collection tool (DCT) was created and trialed in May 2021 over one month and changes iteratively implemented based on suggestions made by the Saturday pharmacist to allow the clinical interventions to be collated more accurately.
- Pharmacists who currently provide the enhanced neuropharmacy Saturday service collected the data.
- The DCT collated information regarding how many medicine reconciliations were completed, how many discharges were drug listed, how many ICU stepdowns were seen and how many interventions were made by the pharmacists whilst on the wards as outlined under the objectives.
- The data from the DCT was then collated on to a spreadsheet and analysed by the investigators.
More Neuropharmacy Academy Service development Projects
Developing neuropharmacists, supporting collaborative care
Knowledgeable pharmacists can initiate or support new treatment pathways, play an important role in patient education, medicine adherence, efficacy and safety, and provide advice to other healthcare professionals involved in the person's care. This Academy recognises the value of this essential role, and seeks to enhance pharmacist's clinical skills and build their confidence in managing a range of neurological conditions.