Safer treatments for hallucinations in Parkinson’s and Lewy body dementia: Parkinson's Cutting Edge Science conference 2022
KnowledgeProfessor Suzanne Reeves, clinical senior lecturer in Old age psychiatry explored safer treatments for hallucinations experienced by people with both Parkinson's and Lewy body dementia.
Suzanne opened her talk by highlighting the way that everyone experiences hallucinations in daily life, such as a shadow twitching which might be initially misinterpreted, or the creak of a door or feeling of a presence which turns out to be the wind or a pet. She explained that these ‘minor hallucinations’ including pareidolia, which is when we see a significance of pattern or facial features in random or accidental shapes, are experienced far more frequently in people with Parkinson’s or Lewy body dementia (LBD) (fig 1).

Fig 1: Suzanne’s favourite example of pareidolia – a face within a fried egg
Major hallucinations are commonly complex visual hallucinations of objects, people or animals, and whilst these can be managed if people have insight into what is occurring, they can become distressing for people who do not have insight, or who are experiencing delusion around the hallucination.
Suzanne discussed briefly the debate around whether Parkinson’s and Lewy body dementia ought to be grouped together or kept separate and outlined the similarity and differences between them. She was clear that the use of DAT scans to ascertain a correct diagnosis is essential due to a person with LBD having a high sensitivity to dopamine d2 receptor agonists, and the majority of antipsychotic drugs are D2 receptor agonists, making them inappropriate to treat those with LBD.
Recognition and assessment
Suzanne explained that appropriately recognising and treating hallucinations in Parkinson’s and LBD patients is essential because of numerous factors (fig 2).
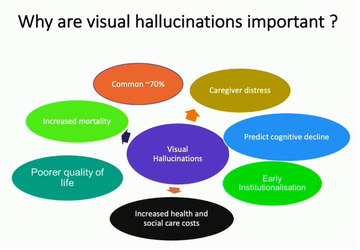
Suzanne’s slide on why it is important to address visual hallucinations in Pd and LBD
Suzanne explained the many complex brain activities taking place in recognising visual stimuli and cues and if any of those processes are not functioning accurately, we can easily misinterpret what we see. She outlined ‘top down’ and ‘bottom up’ interruptions in perception and processing (Fenelon 2012) (fig 3).
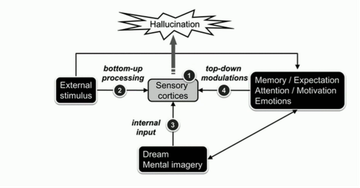
Interruptions in top down and bottom up processes contribute to hallucinations and misperceptions (Fenelon 2012)
De-prescribe before you prescribe
‘Most of what I spend my time doing… is trying to find a way of not prescribing antipsychotic drug treatment, because we know the risks attached.’
Prof Suzanne Reeves
Suzanne explained the various factors to address first as a form of treatment, including:
- Ruling out a physical cause
- Optimising sensory functioning
- Optimising the environment (lighting is key)
- Reduce the impact of symptoms
- Educate carers and individuals to help reduce anxiety and fear around this
She advocated deprescribing before considering prescribing (Friedman et al 2018), specifically, and in the following order:
- anticholinergics,
- amantadine,
- dopamine agonists,
- MOA-B inhibitors
- Finally, and if necessary, consider a reduction in levodopa
Suzanne clarified that, with hallucinations, people are often in a more advanced stage of their disease and that part of the challenge in managing these symptoms is in balancing the discontinuation of medication with the impact of that deprescribing, and the benefit of reducing the hallucinations; these decisions will be made on an individual basis and ideally across a multidisciplinary team.
With a measured discussion of the potential benefits and problems, Suzanne noted that:
- Rivastigmine is usually the firstling treatment for hallucination as it is commonly prescribed for dementia and there is some suggestion that it reduces hallucinations.
- Quetiapine has questionable efficacy but is currently the safest antipsychotic available.
- Olanzapine is not a viable treatment option owing to increased mortality and decreased mobility in patients treated with it.
- Clozapine is the most effective antipsychotic treatment for hallucinations in people with Parkinson’s but is incredibly challenging to both initiate and monitor.
- Movement across the UK amongst healthcare professionals to make this more accessible for use
- Problematic side-effects
Pimavanserin is a potential future option but at present is unlikely to be an option owing to variable success, has high costs and is not yet approved for use in the UK
Discussing her own research into other potential treatments for psychosis, Suzanne highlighted the complex balancing of neurochemistry needed in the brain to ‘see’ clearly and noted the importance of the dopaminergic, serotonergic and GABAergic systems (fig 4).
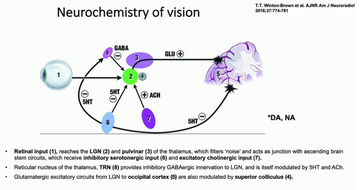
The neurochemistry of vision and new avenues for treatment
Top Hat study
Susanne gave a background to the use of ondansetron, citing both mouse and human studies (Tsitsipa et al 2022) from as far back as 1995 where an open-label trial found considerable promise in the drug as a treatment for hallucinations but did not go to trial owing to high costs (Zoldan et al 1993).
However, Parkinson’s UK have now funded the first Parkinson’s trial of ondansetron, and as PI (primary investigator) of the TOP HAT trial or ‘Trial of Ondansetron as a Parkinson’s Hallucinations Treatment’, Suzanne discussed the trial to date, including the extending of the eligibility criteria to include people with LBD as well.
- Any adult with Parkinson’s or LBD experiencing weekly hallucinations over a 12-week period is eligible to be referred to the trial.
- They have currently recruited 55 people and need 306
- They are particularly looking for new sites in the Northwest of England, where there is a gap at present.
In response to questions from the floor, Suzanne provided measured and thoughtful responses towards questions on some of the current common prescriptions used such as memantine and selective serotonin-reuptake inhibitors (SSRIs). She was clear that whilst they are often prescribed as a 'safe choice' and there is a link between the severity of hallucination and a person's mood, there is insufficient evidence to suggest they are helpful in treating hallucinations.

This meeting is designed and delivered by the Parkinson’s Academy and sponsored by BIAL Pharma. The sponsor has had no input into the educational content of this meeting.
Related articles
'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.


