Before you watch this webinar
Enhancing your learning experience begins with understanding you better. Collecting data enables us to tailor our educational content specifically for our audience. Discover more about how we handle your information in our Privacy Policy.
Event
SPMS: difficult discussions in progressive MS
Our sponsor

This webinar will cover:
- Do we prepare patients for the conversation around SPMS?
- Who should be involved in these conversations?
- When do we tell a patient they have SMPS?
- A look at the variance of treatments offered to pwMS with secondary progressive MS - is it still a postcode lottery?
CPD accreditation
This webinar has been approved by the Federation of the Royal Colleges of Physicians of the United Kingdom for 1 category 1 (external) CPD credit(s). Please note that CPD approval does not include satellite symposia sessions. To claim the credit please email events@neurologyacademy.org.
Prof Eli Silber
Consultant neurologist, King's College Hospital NHS Foundation Trust
Ruth Stross
Director of services, MS Trust
Rachel Dorsey-Campbell
Senior lead pharmacist, Imperial College Healthcare NHS Trust
Presentation slides
Summary
Novartis Pharmaceuticals UK Limited kindly sponsored the webinar on ‘SPMS: difficult discussions in progressive MS’, which was chaired by consultant neurologist Professor Eli Silber, and featured presentations from MS specialist nurse, Ruth Stross, and senior pharmacist, Rachel Dorsey-Campbell.
Eli introduced the session by talking through some of the important questions about how to best care for and communicate with people with MS (PwMS) and went to present the case history of a fairly typical 48-year-old man diagnosed with relapsing remitting MS in 2014, who had had a relapse and been found to have two new cerebral lesions on an MRI scan. Rachel commented that the question of whether this constituted treatment failure was a one that came up in her multidisciplinary team (MDT) all the time; she tended to advise patients that it did not necessarily constitute treatment failure, while some of her colleagues were much more likely to conclude that it did and escalate treatment. Ruth added that she would want to discuss the findings with the patient, along with the impact on the disease on his life and how he wanted to move forward.
Eli presented findings from a French registry study in 200, before the advent of disease-modifying treatments (DMT), which showed that once PwMS reach a significant level of disability (EDSS 4) then the disability progresses at an identical rate in people regardless of the diagnosis.
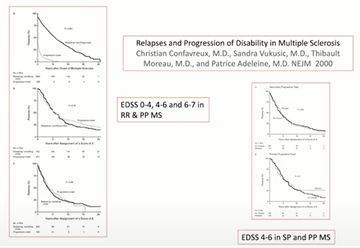
Figure 1
Eli said that he’d continue to treat his patient as having RRMS, as it gave more opportunities regarding treatment, but that he might start thinking about its being transitional disease and start talking to the patients about a gradual build-up of disability. Ruth said that she’s signpost the patient to a good information resource, such as the online patient community, Shift.ms and MS charities.
Eli stressed the need for monitoring PwMS at least one a year, to look for signs of progression, highlighting that Rio and modified Rio scores help to predict long-term prognosis after DMTs have been started. Have we been too nervous to label progression until now, he asked? Ruth commented that this was where an MDT approach was invaluable; the conversation tended to be gradual and ongoing.
The panel went on to discuss stopping therapy for PwMS, based on a second case study - a 58-year-old woman with progressive disability, coming into clinic in a wheelchair. Rachel said that she often raised the EDSS 7 cut-off rule for stopping treatment at MDT meetings and gets pushback regarding the risk of rebound relapse. Ruth raised the issue of patient letters not giving EDSS, and the difficulty with this at the current time [of Covid-19] with remote working. Rachel stressed the need to highlight this problem for the NHS. Eli said we should be doing telephone EDSS, as reasonably accurate outcomes were achievable at higher levels of disability.
Reflecting on the case studies, Ruth stressed the importance of developing a relationship with patients and involving family members. Rachel commented on the value of taking a lead from patients, and all discussed the importance of exercise and activity to counteract deconditioning. HCPs should not get hung up on labels, said Rachel. Ultimately MS is one disease, and our role is to work with patients to help them manage it and live well.
Arguably an advantage of lockdown is that telemedicine may have helped to link us more with patients with secondary progressive MS (SPMS), who can see themselves as ‘forgotten’.
“The ‘forgotten many’ is how people with secondary progressive multiple sclerosis (SPMS) describe themselves. SPMS has a significant impact upon those with the disease, their families, the NHS and society overall”
Gavin Giovannoni
The MS Trust are looking at mapping MS services currently, said Ruth, and this should really help.
Quality of life is fundamentally subjective ‒ and of the seven principles to improve quality of life, patients having a central role in making decisions that affect their care is of paramount importance.

Figure 2
There can be a lot to cover in consultations. Ruth advises patients to write down their questions in preparation for seeing their neurologist. Eli advises medical students that often the most useful question to ask patients is: ‘What do you want from me?’
A 2020 expert panel consensus on SPMS agreed the following actions needed as a matter of urgency:
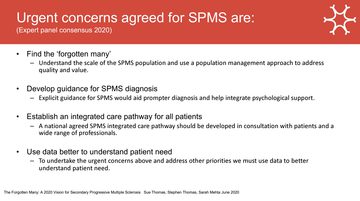
Figure 3
Ruth had found from her own research that around 50 per cent of PwMS may be lost to follow-up. Even in her own community service, they are missing around 20 per cent of patients, notwithstanding efforts to locate them.
Eli’s service has been piloting patient passports for patients with a diagnosis of epilepsy and wondered if this approach might be transferable. Rachel caveated the limited capacity of services to deal with the additional caseload and managing the expectations of patients with SPMS ‒ while Eli highlighted the potential public health benefits, for example, of preventing urinary tract infections and treating osteoporosis in these patients.
Ruth concluded that we need to be improving on the NICE guidance and use the data we have to improve capacity in MS services so that we will be able to cope with these patients when they come looking for MS care. Ultimately, it’s about looking for the ‘forgotten many’.
Additional information
Our sponsor

Encouraging excellence, developing leaders, inspiring change
MS Academy was established in 2016 and in that time has accomplished a huge amount with exciting feedback demonstrating delegates feel inspired and energised along their personal and service development journeys. The various different levels of specialist MS training we offer are dedicated to case-based learning and practical application of cutting edge research.