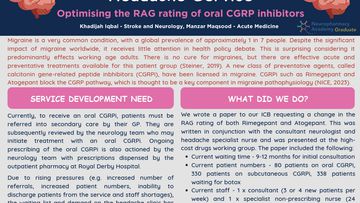
Setting up Specialist Pharmacist clinic for advanced therapies in Parkinson’s disease
Poster
Following a period of observation, the aims of the project were to develop set standards for prescribing specialist Parkinson’s medications, improve documentation and allow audit of the whole pathway. In addition, there was a need to be less reactive to patient requests for medication.
A formulary audit revealed that although using medication appropriately, the target of a clinical review within 3 months of treatment initiation was not well documented in clinical notes.
Further audit of summary care records demonstrated that the advanced therapies were not always recognised on GP systems. As a specialist centre prescribing for patients from a wide geography communication between primary and secondary teams was vital.
Documentation of prescribing as an activity, was improved by the use of simple proformas capturing the clinical review. The proforma also included a series of prompts to ask questions about side effects and obtain blood monitoring information. As a non medical prescriber, building in a process through which I can have defined parameters for practice and later offer a framework for audit, allows some assurance when conducting consultations with complex patients.
The use of an IT patient database allowed the Pharmacist to estimate when a patient was likely running out of medication and be able to contact them rather than the reliance be on the patient notifying the team. This was needed as Pharmacist clinic was only a week.
Unfortunately re-audit was not possible within the project timescale but it is planned and expected to show improved standards of documentation in the use of advanced therapies.
This project targeted some of the difficulties identified with a service managing patients with complex needs and the actions taken so far have gone some way to tackling them. Further work is planned to improve the patient experience.
Aim
To develop and agree standards, pathways and associated support for use in a specialist pharmacist clinic for the prescribing and managing of advanced and specialist therapies for Parkinson’s disease, namely Duodopa, Apomorphine and Safinamide.
Headlines
A new pharmacist clinic was established in Dec 2020 to support the NBT Movement Disorder Team (MVD) in prescribing and managing advanced and specialist therapies for the treatment of Parkinson’s patients across a growing number of patients across a wide geographical area.
Through evaluation of the service, a previous audit of Summary Care Records and an internal audit of Safinamide prescribing was considered together.
Key findings
There were no standard parameters by which to manage ongoing ‘red’ drug therapy; with ractive requests for repeat prescriptions often outside of clinic times
Bloods results and tests could not always be located in electronic patient records
Primary Care often did not hold records of these medications
Although treatment was initiated for Safinamide as per local formulary guidelines, only 55% of patients had a documented review within 3 months and in less than 20% of cases efficacy was clearly documented.
Changes to practice made
This service development is ongoing. To date the initial objectives have been achieved:
Clarification of the patient pathway after Consultant starts new therapy
Agreed monitoring standards for each medicine
Use of a standardised prescribing proforma to document clinical review
The IT solution allows prescribing to be planned and is now being used, (although due to the volume of patients on each therapy it will take some time to be fully built.)
Core recommendations
Develop patient-facing information to help reduce this risk,
Extend this work to a national level.
More Neuropharmacy Academy Service development Projects
Developing neuropharmacists, supporting collaborative care
Knowledgeable pharmacists can initiate or support new treatment pathways, play an important role in patient education, medicine adherence, efficacy and safety, and provide advice to other healthcare professionals involved in the person's care. This Academy recognises the value of this essential role, and seeks to enhance pharmacist's clinical skills and build their confidence in managing a range of neurological conditions.