Key highlights from ECTRIMS 2024
KnowledgeThe 2024 European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS) Congress took place in Copenhagen, Denmark, blending both in-person and virtual participation to bring together a diverse community of researchers, clinicians, healthcare providers, MS organisations, and individuals living with multiple sclerosis (MS). This year’s congress theme, “Celebrating 40 years of dedication to MS research and treatment”, highlighted four decades of breakthroughs and ongoing efforts to improve MS care.
As always, the congress featured an impressive lineup of keynote speeches, scientific presentations, educational sessions, and more, including a dedicated patient community day. These sessions explored cutting-edge research and treatment developments, with a particular focus on remyelination and new therapies aimed at repairing myelin, the protective sheath damaged in MS.
Updated McDonald criteria
The McDonald criteria for MS are regularly updated on the basis of new evidence to allow an earlier and more accurate diagnosis of MS. The 2024 revisions of the McDonald criteria represent a sea-change in the approach to diagnosing MS. Some key elements including the need for a “typical” clinical syndrome, the requirement for dissemination in time and separate diagnostic criteria for relapsing and progressive MS have been removed. A number of new diagnostic biomarkers have now been incorporated into the MS diagnostic criteria including central vein sign and paramagnetic rim lesions on MRI, kappa free light chains in the CSF (as an alternative to oligoclonal bands), and optic nerve assessments with MRI, VEPs or optical coherence tomography. These biomarkers hold promise in aiding in MS diagnosis but whether they can be widely adopted in the NHS remains to be seen. The MS Academy will be developing educational webinars around these topics in early 2025.
CAR-T cells
There was a lot of buzz at ECTRIMS 2024 about CAR-T cells, a transformative treatment for haematological malignancy that is now being tested in patients with autoimmune diseases. This “one and done” approach to treating MS hopes to eradicate pathogenic lymphocytes in the periphery and trapped within the central nervous system. Early phase trials are now underway to test the feasibility and safety of CAR-T cell therapy in MS, including in the UK led by honorary academic director and consultant neurologist Dr Wallace Brownlee.
Progressive MS - success and failure
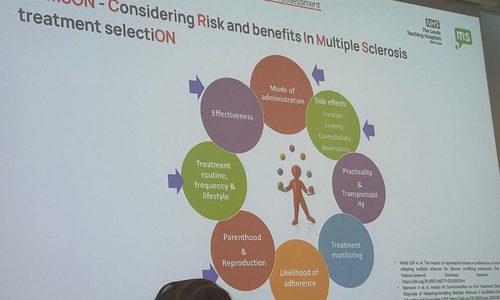
BTK inhibitors have been an area of great optimism in the MS field given their potential to target both the peripheral immune system and compartmentalised inflammation in the brain, one of the important mechanisms driving disease progression in MS. Hopes were dashed by the negative trial of evobrutinib in relapsing MS announced in December 2023. A similar trial of tolebrutinib in relapsing MS presented at ECTRIMS 2024 also failed to meet its primary endpoint of a reduction in annualised relapse rate compared with teriflunomide. However, a trial of tolebrutinib in non-relapsing SPMS patients showed significant slowing in the rate of disability progression compared with placebo, although like in other trials there were concerns about liver toxicity. The UK-based phase III study of high-dose simvastatin in SPMS led by Prof Jeremy Chataway was also presented at ECTRIMS 2024 as a late-breaking abstract. Simvastatin showed no benefit on disability progression compared with placebo over 3 years, although many secondary endpoints including MRI are yet to be analysed. Nearly 1000 people with SPMS in the UK took part in the trial and the results will be a huge disappointment to people living with progressive MS, and for research teams around the country who worked hard to deliver the study, particularly over the COVID-19 pandemic.
UK Women in Multiple Sclerosis (UKWIMS) group
Agenda setting pre and during clinic appointments
Ruth Stross, Dr Kate Petheram and Dr Ghaniah Hassan-Smith, MS Leaders Academy MasterClass project
The UKWIMS group led by Dr Tarunya Arun held a meeting to network, support and collaborate with each other. The meeting room was packed with neurologists, nurses, neurophysiotherapists, clinical and research colleagues, MS charities and people with MS. The topic discussed was around ‘Agenda setting’ pre and during clinic appointments. This generated an energetic and interesting discussion around how best clinicians can utilise valuable time in the clinic to ensure the patient and clinician agendas are acknowledged and time allocated to both.
Ruth Stross, Dr Kate Petheram and Dr Ghaniah Hassan-Smith presented on the topic with other delegates in the audience including Rachel Dorsey-Campbell, Dr Bindu Yoga and Andrea Stennett. The MS Leaders Academy recognised the constraints of current services and the wider challenges facing the NHS, so for their project they decided to focus predominantly on the concept of individualisation, specifically considering how they could make services more patient-centred, closer to home, equitable, and able to link between services. The result was to develop 'My MS Agenda', a patient-led, pre-consultation tool (Evaluation of MS Leaders Academy 2023). This would be shared with people with MS prior to a routine consultation and used to steer and frame the discussion at the appointment.
The MS Leaders Academy equips clinicians with the skills, tools and confidence to lead change both locally and nationally.
Delegate feedback
Agenda setting in healthcare appointments is a communication strategy that involves establishing a list of topics to be covered at the beginning of a visit. It is a collaborative process between the patient and clinician to establish a shared focus for the conversation and working relationship.
Agenda setting is considered best practice and is used by psychologists routinely in their practice. It is thought to improve patient outcomes and experience, as well as physician organisation and time management.
Some benefits of agenda setting include:
- Reducing surprise topics
Agenda setting can reduce the number of unaddressed concerns and "surprise" topics that patients introduce later in the visit - the “door handle” moment where the person’s top concern is only raised at the end of the visit.
- Improving communication
Agenda setting can improve communication between patients and physicians, which can lead to better adherence and clinical outcomes.
- Establishing a collaborative environment
Agenda setting can establish a collaborative environment where the patient's opinions and input are welcomed.
There was so much interest and energetic discussion around pre-clinic and during clinic agendas, predominantly the patient and clinician agendas and how to align both to ensure patient care is optimised, up to date, safe and MS teams are supporting self management and self efficacy. There will be a follow up meeting to discuss next steps with those already involved and others who may be interested.

Ghaniah Hassan-Smith, Kate Petheram and Ruth Stross presenting at the UKWIMS meeting ECTRIMS 2024
Slides: Agenda setting
Menopause poster at ECTRIMS
Stross et al
A collaboration of MS health care professionals have been looking at personal and clinicians experience of MS and menopause. They first met in January this year and brought a poster to ECTRIMS highlighting their work so far titled ‘Optimising menopause management in MS through multi-stakeholder collaboration and pathway development’
Menopause marks a significant transition, with considerable biological, social and psychological impacts. The impact of menopause can be further complicated for those living with a long-term condition such as MS. Many women face difficulties in distinguishing signs of menopause from their MS, relying on healthcare providers for both clarification and effective management. Increased public awareness of the menopausal transition has led to better awareness of symptoms and treatment options, but it is crucial that services are well-designed, resourced and informed to meet public expectations. To identify the needs of women with MS and their healthcare providers around menopause and MS. To collate ideas on priorities for improving education, pathways and collaborative working, in order to enhance care across primary and secondary care settings.
The group had a combination of information gathering via focus groups and service pathway mapping.
They explored key questions around the experience of menopause with women with MS who are currently or who have recently experienced menopause. Alongside this they collected examples and feedback on how the crossover of care between primary and secondary care has and has not worked. They used this to explore ideas on how this can be improved and where priorities should lie.
They also met with healthcare professionals involved in supporting women with MS to discuss perceptions of their current role in this pathway, their level of knowledge, interprofessional relationships across primary and secondary care, existing crossover or failures of care and key priorities for improvement.
The group used this combined evidence to highlight red flags where gaps in services or education exist, suggest areas for improvement, and key priorities to be taken forward for both patients and healthcare professionals.
This scoping work has informed development of a current best practice integrated care pathway as well as a longer-term optimal and aspirational care pathway. These will then be used to influence policy developments within both MS and menopause focussed initiatives.
Poster: Optimising menopause management in MS
Self-management and self-advocacy: super power to empower
Fiona d’Young MS specialist nurse, New Zealand

So much around brain health encompasses self-management. For further reading, Prof Gavin Giovannoni’s article on self-management provides an excellent resource. Fiona talks through self-advocacy as the ability to recognise, understand, and effectively communicate one’s own needs to other people, including friends, family members, social workers, in the work environment and health care professionals. Being an advocate for yourself means being actively involved in getting what you need or want. These are our superpowers.
With the advent of the smartphone, there are now apps and lots of content available. Here are some mentioned in the session for people with MS and healthcare professionals:
Menzies university training programme - recommended: Resources | Multiple Sclerosis Society of NZ
Cando - Canadian based online platform for MS which includes coaching Coaching - Can Do MS
Dr Sally Shaw, Dr with MS, podcast ‘But you look so well’ (CEO of their own healthcare) But You Look So Good | podcast on Spotify
MS translate - Drummond brothers - translates the academic work into podcasts MStranslate
MS Selfie - Gavin Giovannoni - designed pwMS the confidence to make decisions about their care MS-Selfie
Shift.ms - social network for pwMS to connect MS Support | The Buddy Network
MS together - UK based social network 18-35 yr old MS Together
theMSguide.com blog Dominic Shadbolt
'Living Well with Multiple Sclerosis' podcast | Overcoming MS
Lastly, one of our own pieces of online education for healthcare professionals: Supported Self-Management in Multiple Sclerosis | Neurology Academy

Fiona d’Young, MS specialist nurse, New Zealand, ECTRIMS 2024
Brain health - time matters 2024 report
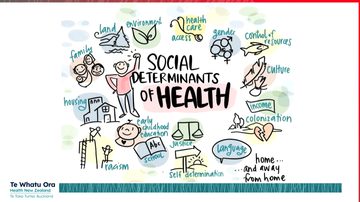
These are encouraging pwMS to ‘lean in’ to be more supported, it doesn’t feel comfortable and is sometimes lonely, but as long as the services are designed to listen and hear and support. Fiona mentions the importance of acknowledging the social determinants of health, we must consider all of the barriers to engagement. MS nurses are well placed within our role to advocate for pwMS. The MS specialist nursing role has existed for over 20 years. The updated Brain health – time matters report summarises parts of their essential role in care; providing education, counselling and assistance navigating complex health systems and supporting lifestyle changes. The report also highlighted that although the benefits to patients having access to a specialist nurse, in high-income countries there are 0.4MS specialist nurses per 1000,000 people, falling to 0.1 per 100,000 people in upper-middle income countries and with none reported in lower-middle income countries and low-income countries.
Fiona highlighted some barriers to self advocacy in women with MS:
Family - lack of support, parental fear for child’s future, non-acceptance
Employment - lack of job security so less able to advocate for altered job space
Medical - distrust of neuro team, economic, physician environment
Environmental - geographical
Sociocultural - stigma, judgement and shame
Psychological - inadequacy, pessimism
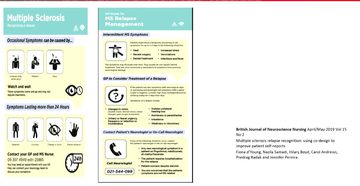
She mentioned the importance of health service codesign, improving services in conjunction and partnership with pwMS. This led to collaborative work which is published in the BJNN around co-design of information in managing relapses (figure below). Multiple Sclerosis Relapse Recognition: Using Co-Design to Improve Patient Self-Reports | British Journal of Neuroscience Nursing
Barriers to self advocacy and self-management
Joelle Massouh, MS nurse manager, Lebanon
Joelle discussed the barriers to supporting a pwMS to support their own self-management linked closely with the social determinants of health. Also a reminder for clinicians to allow the person to take the lead rather than make decisions on their behalf. Again a reminder to listen and let the pwMS to set the clinic agenda as mentioned above.

Joelle Massouh, speakers' slide
Linking self-advocacy and self-management in MS to the MS nurse competency document
Mavis Ayer, lead MS specialist nurse, Southampton, UK
Mavis, previous co-chair of the UKMSSNA gave an insightful talk on how the MS nurse competencies encourage self-advocacy and self-management for people with MS. The Multiple Sclerosis Specialist Nurse Competency Framework is available here for all new nurses and allied health care professionals, it provides a structure to learning, encouragement on achievements and ensures all areas are covered.


Fiona d’Young, Joelle Massouh, K-J Lazarus, Ruth Stross, ECTRIMS 2024
Reflections on ECTRIMS and the 1st Patient Community Day
written by K-J Lazurus, MS nurse specialist, Melbourne, Australia
What a privilege it was to be able to attend ECTRIMS 2024. To be surrounded by the Dedicated to the Dedicated, all these HCP’s and scientists striving to make the lives of those living with multiple sclerosis (MS) better, by looking, asking, networking and researching in so many areas.
The program was packed full of so many presentations covering not only MS in both adult and paediatric populations, but also NMOSD and MOGAD was greatly reflected at this year's meeting. There was so much on offer, making it impossible to attend all the sessions of interest, but despite this, there were many things to be learnt and shared.
Whilst there were so many takeaways from this meeting, I found there seemed to be a common theme through many of the presentations I attended, and that was the importance of Brain Health. Brain health being the lifestyle changes or disease modifying behaviours (DMB’s) that people living with MS (plwMS) can implement to help them live well with a MS diagnosis. There seems to be some shift from a purely medical model focus to a now a stronger focus on the biopsychosocial context.
Key elements of brain health included, but not limited to, healthy diet, regular tolerable exercise, don’t smoke, limit and/or manage vascular risk factors, keep an active mind, psychological support and good sleep hygiene. Managing aspects of one’s overall health continues to show, in many areas of research, better outcomes and quality of life for those living with MS.
It was great to see this year there were two nursing sessions, filled with nurses who did an exceptional job of representing their important roles and work from many corners of the world. They presented their expert knowledge and experience around brain health and self-advocacy, presenting their passions, hard work, research and co-design projects and experiences.
Patient Community Day and interactive sessions, written by K-J Lazarus
This year ECTRIMS also further developed their Patient Community Day, which was held just a few short hours after the official closing of the ECTRIMS Conference, at the Conference Centre in Copenhagen. There was an impressive turnout of over three hundred attendees in the auditorium, along with many more (around 2000) who had registered online, who had gathered in anticipation of hearing the latest updates from the conference. There were translation services available for anyone who was in need of them. And I heard that in some areas of Europe viewing parties were held! ( I pictured something like Eurovision)
The session had two back to back panels, with much to discuss, delivered by expert international panelists that included several specialist neurologists, plwMS and NMOSD, nurses, director of the Danish MS registry and the CEO of the National MS Society of the US.
In the first panel, the topics covered were remyelination, breaking news update on tolebrutinib study, risk factors, symptom management and lifestyle modifications.
The attendees were initially provided with information about the current focus on remyelination, as the new frontier in the treatment of MS. There is much research going on in this space, so news to come in the not too distant future.
It was then acknowledged there are still no currently available treatments to manage disease progression, however there was late breaking news, just earlier that day, in which the tolebrutinib trial (HERCULES) showed a decrease in disability accumulation in non-relapsing secondary progressive MS. It did not, however, meet any of the endpoints in people with relapsing MS.
In other breaking news at ECTRIMS, it was unfortunate it was found that use of statins had no effect on slowing down disease progression.
There was then a discussion around symptoms management and trying to find better strategies to improve quality of life measures such as fatigue, cognition, mental health and continence function. There is ongoing emerging evidence of the importance of brain health strategies with lifestyle modifications, in this area. Explained from a “What Can I Do?” perspective, making positive changes in diet, exercise, controlling vascular risk factors just to name a few, there can be improvements in QoL measures, better enabling living well with MS. Even one small step can lead to bigger steps with better quality of life outcomes, and this can be further assisted with integrated health care teams, where possible/available.
Along with this was a consideration of a need for a better understanding about diversity in MS, around age, especially in the under 18 yo and over 65 yo’s, race, gender, ethnicity and social circumstances to be undertaken globally. Discussion was had around clinical research cohorts don’t often reflect these population differences, and how to remedy this moving forward into the future, to be more inclusive.
The second session covered the incoming new diagnostic criteria, paediatric MS, the role of the MS nurse and update on NMOSD and MOGAD.
The importance of the evolution of the diagnostic criteria, with some preliminary discussion around the pending changes (as they are still awaiting peer review) will lead to an enhanced path to a diagnosis of MS. With the improvements in MRI technology, the increased understanding of biomarkers and now likely inclusion of changes in the optic nerve which should decrease the risk of misdiagnosis and decreased time to diagnosis, allowing for more rapid management to be put in place.
There was quite some focus this year on paediatric MS, and how they are often an underrepresented group of plwMS. It was acknowledged is more of a rare disease in this age group of under 18 years, that presents somewhat differently, and symptoms can be different, there should still be some urgency that they have access to effective treatments. There is also some potential that there can be valuable information gained from this group by looking into early remyelination, as cognitive changes are different in this group. New research guidelines and protocols need to be considered, and promptly in this population. It was also noted the importance of the role of the nurse in the paediatric space to support the patient, but also the family of the patient, as this can be a complex and timely factor of paediatric MS care.
The role of the nurse was then covered, with a reflection of an Australian MS nurse study showing there were better outcomes in pwMS that had access to a MS nurse, and this increased the longer the relationship with the MS nurse. The context of accessibility to MS nurses around the globe was noted as an area of need for further development and support.
The opportunity of networking at ECTRIMS 2024 with many of the international MS nurses was noted as a key opportunity to allow for collaboration and to build relationships to look at ways to improve some of the global gaps.
K-J Lazarus
Long term relationships with MS nurses offer continuity of care, not just at a time of intervention or times of urgent need, but they also provide a specific skill set and understanding of a complex medical condition with many complex needs. They are able to provide tailored individualised collaborative care to plwMS, coaching around living well with MS by providing support and understanding of brain health and lifestyle modifications, how to effectively self-advocate and self-manage to promote positive changes.
There was also representation in the audience from plw NMOSD/MOGAD, and the increased information available at this ECTRIMS was applauded and discussed how this might be used moving forward, to further develop treatments, and management protocols for the future, with much more understanding to come.
There was some time for questions from both the online audience and of those present in person, that reflected a keen interest in the latest news to come out of the conference. I am sure the Patient Community Day will become a regular fixture of the ECTRIMS Program, with plans already being considered for Barcelona 2025.
The other personal highlight for me, due to attendance at ECTRIMS is a very rare and valuable opportunity, I was able to meet, share and learn with other Nurses from around the world, that I would not otherwise get the chance to meet and collaborate with. From the new and some old friendships and alliances built at ECTRIMS 2024 I am excited to see what opportunities that may come as a result of our meeting, sharing of ideas, and all working towards the same goal of caring for plwMS and other like neurological conditions, enabling improved QoL markers for them, of their doing and choice, in all communities across the world, where possible. It just needs to start with one small step!
K-J Lazarus
Shift.ms session: The MSer experience: risk every way i turn, Roxy Murray
It was good to meet Damian Washington who chaired this session, and hear Roxy Murray’s honest account of her experiences with MS. She complimented the role of the nurse and said this had been a key role during her journey with the disease, this was someone who would give her time and listen.
By way of summary here is the ECTRIMS official wrap-up video:
Related articles
Encouraging excellence, developing leaders, inspiring change
MS Academy was established in 2016 and in that time has accomplished a huge amount with exciting feedback demonstrating delegates feel inspired and energised along their personal and service development journeys. The various different levels of specialist MS training we offer are dedicated to case-based learning and practical application of cutting edge research.