Our first ever national neurology transformation meeting
NewsOn 31st January, we welcomed more than 120 commissioners, managers and clinical leaders across the NHS to Birmingham for the first national neurology transformation meeting.
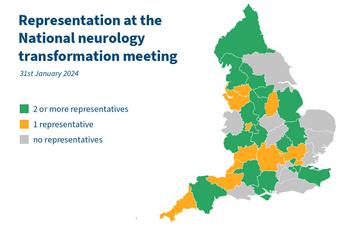
We were thrilled to have representation from all but seven of the country's integrated commissioning boards (ICBs) registered at the meeting, whilst a few additional attendees on the day shared that they were from a 'red' region, giving us exceptional representation (fig 1). Almost 50% of attendees were healthcare professionals looking to work with service planners and commissioners to transform neurology services for the future, whilst the other half of attendees were the managers and commissioners themselves.
Figure 1: Representation by integrated commissioning board (ICB) region registered for the National neurology transformation meeting on 31st January 2024
We developed the meeting in partnership with NHS England's national clinical director for neurology, Dr Niranjanan Nirmalananthan and clinical adviser for the NHS England neurosciences transformation programme Dr Martin Wilson with a key aim: to provide practical information and insight into the transformation strategy. The meeting's goal was to identify challenges, consider solutions, learn from existing whole-system services, and develop networks - and it did it in spades.
We decided to distil some of the key messages down for a clear and succinct summary - so here are some of the speakers' core insights, transferable learning and recommended tools to progress neurology services in 2024 and beyond.
Feedback
92% of delegates rated the meeting as 'good' or 'excellent' across three core themes: 'overall relevance to educational needs', 'overall quality of education offered' and 'effectiveness of the course for your professional development'.
'I think the whole day was excellent; I would 100% attend again. I have gained lots of insight and information on things I had never thought about and I am hoping to start looking at themes I will be able to bring into my service and clinical practice.'
'All speakers were fantastic and added very useful and thoughtful aspects to take back to our areas. I liked the view of the patient voice being noted in any improvement process.'
Comments from delegates post-event via evaluation form
One of the key messages from commissioners themselves to clinical leaders was this:
Create and present credible plans and solutions for commissioners rather than highlighting problems or needs.
Key challenges identified:
During the meeting, the challenges facing the NHS generally, and neurology specifically, were openly discussed. However, for the majority of challenges, opportunities or solutions were also presented. These challenges included financial scarcity, the ageing population, a stretched and depleted workforce,a growing treatment landscape, areas of significant deprivation, and widespread variance in both service availability and equity of access.
'The NHS financial climate is not amenable to transformation.'
Dr Andrew Kelso
Georgina Carr shared results of the 2022 My Neuro Survey, highlighting huge variance in experience from personalised care and consistent support, to challenges in access and a feeling of being lost to the system:
1 in 5 adults had to wait more than 12 months for a referral from their GP to see a neurologist
40% are not being referred to key services such as physiotherapy, often because the services are not there
45% of people felt that post-inpatient stay, there was insufficient care offered to rehabilitate them
85% of children and young people had not been offered a named keyworker, despite NICE guidance calling for this as standard.
'We want to deliver an integrated care solution for neurology, thinking - not only about the people at your door - but every person in the population who might be struggling to access services.'
Dr Niranjanan Nirmalananthan, national clinical director neurology & consultant neurologist
Key solutions offered:
A number of solutions were offered from systemic change like 'the left shift' and widespread collaboration across health, social care, the voluntary sector and patients themselves in equal partnerships, to working differently, maximising resource and team skillsets, adopting new service models, and consistently learning from others' experiences whether formally or informally.
Andrew presented the idea of 'the left shift' which he feels is applicable to every condition and area of care. Demonstrating how shifting patients to the left from each segment of care (see figure), he explains the positive impact this can have for both the patient and the NHS (NHS Confederation 2023).
'We want to keep as much care as possible to the left, ensuring more patient-centred care, closer to home.'

'A strong ICP has representation across health, social care, voluntary sector and patients themselves.'
Figure: A successful ICP

Throughout the conference, the delegates heard of Pathfinder projects, services adopting a whole-system approach to provision and care, and were encouraged to learn from these and consider how they might be applicable to their own locality or services.
Dr Fiona McKevitt, clinical director for outpatient recovery and transformation at NHS England, consultant neurologist at Sheffield Teaching Hospitals NHS Foundation Trust and an honorary senior lecturer, talked through the issues that have been facing outpatient appointments for years, and the changes that have been made more recently, and suggested a whole host of different solutions based on learning from different parts of the country.
Figure: 'A busy slide' looking at successful changes to outpatient appointments from sites across the UK
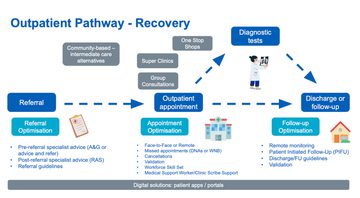
Successful changes to outpatient appointments from sites across the UK
Follow up optimisation can include:
developing clear discharge guidelines,
making use of remote monitoring
offering patient-initiated follow-up (PIFU)
Appointments themselves can be optimised through:
reviewing and changing the consultation modality to suit the need,
addressing missed appointments - finding out the core reasons they occur in your locality or key patient groups and getting the the root of the problem as well as making cancellation or change of modality an easy option:
- offering an emergency cancellation number or direct access contact
- calling the 'missing' patient directly and conducting the appointment on the phone
- providing innovative clinic solutions
- e.g. one stop shops (optimising both patient and clinical time) group consultations
- super clinics (where a senior clinician overseeing multiple clinics each run by an individual team member).
Shelley Jones, consultant pharmacist: neurosciences and deputy chief pharmacist for transformation and systems integration at King's College Hospital NHS Foundation Trust gave a message of hope and optimism. Presenting how the new changes in delegated budgets affect high cost and highly-specialist drugs by demystifying what these are and how they are - and will be - delivered, she highlighted a number of challenges which may be overcome through delegated budgets whilst acknowledging a number of new problems which may arise as a result.
'By making it local, we will be able to deliver better services, without losing that national oversight that ensures they are safely delivered in line with guidance.'
Shelley Jones
Ultimately, though, Shelley suggested that rather than trying to shoehorn existing systems into the new ICB structures, this is an opportunity to create bespoke solutions and design new pathways. She advocates for getting financial services to engage in the design decisions to ensure the funding flows properly and with minimal stalling or hurdles.
Tools to support transformation:
A range of tools were presented to help facilitate and support neurology transformation, from optimal pathway blueprints and example projects around the country, to technology aids like data dashboards and online collaboration tools.
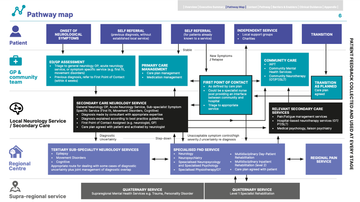
Georgina introduced the optimum care pathways (OCPs) as a tool to compare a current service to an optimal one. The OCPs can help services to identify good practice to maintain or extend, analyse gaps, locate challenges, identify opportunities to use workforce or resource differently, as well as to frame services within national policy and guidance.
Figure: Example pathway map from Optimum clinical pathway for adults: Functional Neurological Disorder p6
Another tool presented was the brand-new neurology data dashboard. Dr Martin Wilson, consultant neurologist, chief clinical information officer (CCIO) at the Walton Centre NHS Foundation Trust, and clinical adviser for NHS England's neurosciences transformation programme shared static screenshots of the new tool. He explained how it can be used to gather information on equity of access across a whole ICS, both in-patient and outpatient metrics, flows into and out of an ICB, cost effectiveness, and benchmarking.
Figure: A screenshot of the adult neurology ICB dashboard
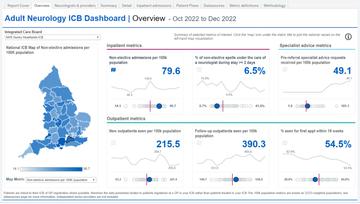
It is hosted on the national clinical data repository (NCDR) and requires an Octa account to sign up.
Lucie Waters, director of the South London Office of Specialised Services, discussed how specialised budgets will be delegated and the benefit that this will have in bringing integration to the whole of the patient pathway - and used a number of Pathfinder sites to bring this to life. Pathfinders around the UK are employing whole-system transformation to a specific service or pocket of care to foster learning and enable its translation to other sites, services, or broader transformation.
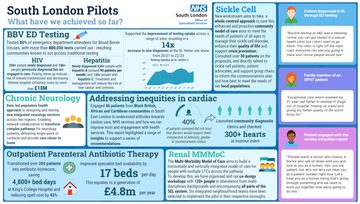
From initiating a community care model to the previously 'specialised' sickle cell service, to a new neurology pilot crossed Southwest London and Surrey Heartlands, the examples she gave had all employed the 'left shift' that Andrew Kelso spoke of to some extent, with the neurology pilot deliberately planning change at each level of care to propel that same shift.
Dr Fiona McKevitt, noting the benefit of Pathfinder sites as well, also introduced the FutureNHS tool, an online collaboration platform available across health and care agencies at no cost to support and facilitate information sharing, planning, and general cross-working through online communities, workgroups and shared boards.
Worried you've missed out?
We know live attendance isn't possible for everyone, so we recorded all of the presentations to make sure the content would be available to any who need it. We're pleased to offer free access to every session via our online learning portal. All you need to do is fill out the registration form on the event page, and you will have access for a 12 month period. Meanwhile, if you did attend and want to watch back some of the talks you found most impactful, pop to your log-in area - they're all waiting for you!
Documents to support insight:
Neurological Alliance, Together for the 1 in 6: UK findings from My Neuro Survey 2021-2022 accessed via https://www.neural.org.uk/wp-content/uploads/2022/05/Together-for-the-1-in-6-UK-Findings-from-My-Neuro-Survey-v6.pdf
Fuller G, Neurology: GIRFT programme national speciality report, September 2021, accessed via https://gettingitrightfirsttime.co.uk/medical_specialties/neurology/
NHS Confederation, 'The link between non-acute investment and system productivity, September 2023, accessed via https://www.nhsconfed.org/system/files/2023-09/The-link-between-non-acute-investment-and-system-productivity%20.pdf
Royal College of Physicians, Outpatients: the future – adding value through sustainability, 9 November 2018 accessed via https://www.rcplondon.ac.uk/projects/outputs/outpatients-future-adding-value-through-sustainability
NHS Improving Quality, The new era of thinking and practice in change and transformation: A call to action for leaders of health and care (2023) https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2018/09/Change-and-Transformation-White-Paper.pdf
The meeting was made possible through funding from a range of pharmaceutical partners: Roche Products Limited, argenx UK Ltd, Novartis Pharmaceuticals UK Limited, Pfizer Limited, Merck Serono Ltd., and Sanofi. None of the sponsors had any control over either the organisation or educational content of the meeting.
A few photo's from the day:
Related articles
Uniquely practical education, producing specialist clinical leaders transforming local healthcare
Neurology Academy is an innovative educational provider for healthcare professionals including consultants, specialist nurses, pharmacists, therapists and other allied health professionals. Our courses are developed by practicing specialists who combine their experience and expertise into case-based learning designed to create specialists in their field with confidence in effecting change.














