Movement disorder service Royal Alexandra Hospital: Are we meeting our population need?
To plan further development within a service, or indeed determine need for development, I feel a sound knowledge of current practice is required. I chose to look at our movement disorder service within the Royal Alexandra Hospital (RAH) Paisley to ask the question: do we have capacity to meet our patient population’s need?
The RAH is a district general hospital within the West of Scotland and is part of the Greater Glasgow and Clyde Health board. We cover a mixed urban rural population. Currently there are two consultants with a movement disorder interest and a Parkinson’s Disease Nurse Specialist (PDNS). There are three movement disorder clinics a week supported by an additional day hospital resource.
Methods
Establish population
I utilised 2011 census data to confirm the population served by the RAH outpatient department. The census Scotland website offers a variety of ways to interrogate population data e.g. by post code, local authority or even health board. I chose to search using a combination of local authority and post code data.
Prevalence of Parkinson’s disease
SIGN 113 “Diagnosis and pharmacological management of Parkinson’s disease” quotes prevalence of PD at 120 to 230 per 100,000 population. I hoped to narrow this range down. Newman et al comment on higher than expected variability in prevalence in the West of Scotland in their paper “Geographical difference in Parkinson’s disease prevalence in West Scotland”. The prevalence will of course vary according to age demographics. The Aberdeen PINE study state prevalence lies between 160 to 180 per 100,000 and this is the range I chose to utilise.
Patient data
Using our IT system TRAKCARE I collected the CHI number of every patient attending the three movement disorder clinics from August 2016 to August 2017. All CHI data was entered into an excel worksheet and duplicate attendances eliminated to establish patient numbers. I then reviewed all patients‘letters to establish diagnosis and staging of Parkinson’s disease.
Results
Using methods described above I established the RAH out-patient population is currently 197,672. A range of 160 to 180 per 100,000 would predict we should care for 316 to 355 people with Parkinson’s disease in our service.
Analysis of actual patient numbers confirmed 384 people attended the 3 clinics in the year. Clinic split 130 new to 752 returns.
Not all of these 384 patients however are diagnosed with Parkinson’s disease.
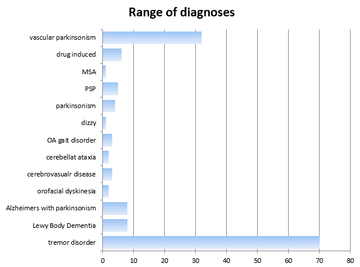
The following chart demonstrated the range of diagnosis.
After eliminating the above cases I established 239 patients with Parkinson’s disease currently attend our service. The clinic letters suggest of those 239 patients 8% are at diagnostic stage, 50% maintenance, 37% complex and 5% palliative.
This number falls short of our 316 to 355 expected. Our hospital however geographically sits very close to the Queen Elizabeth Hospital in South Glasgow. This is relevant as the neurology institute is situated here. Historically our neurology colleagues have accepted patients from our catchment area, particularly those of younger years.
A request for patient attendances at the neuro-institute confirmed 104 RAH patients receive their PD care under the neurology team. Of interest to me however, was the breakdown of those numbers, revealing last year my neurology patients saw 4 new RAH referrals and 91 returns (the remainder were DNAs). Of course, the patients who receive out-patient care through the Queen Elizabeth would still be admitted to the RAH if in-patient care is required. It is therefore vital we establish good ties across these sites.
The number of people therefore in our catchment area with a diagnosis of Parkinson’s disease is 343, which sits within my predicted range.
Our service has participated in the PD audit this year and we hope to get feedback through PREMS relating to our patients’ experience at clinic
Conclusion
My analysis would suggest that at present we offer a good service to our patients, in that most are seen at least twice a year. The patient perspective is vital and work is underway to evaluate this further.
Of note is the low number of new referrals seen through the neurology service last year. It seems my neurology colleagues are starting to divert vetting of RAH patients to the local service now. Anecdotally that fits, as within our service in the last years, we have seen a steady increase in the time patients have to wait for first assessment, reflecting an increase in new referrals.
I hope that this data would be useful in the justification of increasing sessionary commitment to our movement disorder service. This would allow us to continue to meet our population demand and avoid breeching waiting times for first reviews.
As noted above I feel it vital to forge links with our neurology colleagues as we will undoubtedly share patients over time. Our local neurologists have now established a regular movement disorder video meeting where we come together to discuss diagnostic uncertainty and complex cases. Our team will endeavour to contribute to this group.
I now have CHI data for our current case load. There is a local initiative in Greater Glasgow and Clyde using our IT system TRAKCARE. Our patients with Parkinson’s can have an alert tagged to their electronic records, which will trigger an email to nurse specialist when and if those patients are admitted to hospital either for elective or emergency care. The hope being, the movement disorder team can be pro-active in offering advice, particularly relating to medication and nil by mouth policies if relevant. I can use this data to identify our service users.
I have found this exercise to be particularly useful to gain a clear understanding of our population numbers and perhaps now plan better for the future. I next plan to expand this body of work to look at the Clyde sector as a whole.
More Parkinson's Academy Service development Projects

'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.