The Introduction of a new model of care using telephone appointments prior to face to face review for newly referred patients to a Medicine of the Elderly Parkinson’s Service
Poster
Background
New patients in our Parkinson’s Service have previously initially been reviewed with a one-hour telephone appointment. However, as a result of the COVID 19 pandemic, we had to undertake telephone appointments to satisfy restrictions, with some positive effects demonstrated, particularly with regard to patient and carer satisfaction. (1) Face to face clinic (F2F) appointments have gradually been re-introduced and we are now seeing the majority of patients face to face. Due to social distancing, we have tried to reduce the time that patients spend in, or waiting, at clinic. As we have identified benefits from telephone consultation when it has been necessary, we thought it may be useful to trial a telephone consultation for new patients, prior to face-to-face clinic appointment to introduce the clinic, gather history, introduce some possible diagnoses and order tests in advance. This fits with current Scottish Government guidance regarding Active Clinical Referral Triage (ACRT) and we hoped it would increase efficiency and be beneficial to patients.
The Liberton MOE Parkinson’s service covers a large geographical area, serving a total population of approximately 348, 000. The service accepts referrals from a number of sources including General Practice, other hospital consultants, neurology patients with an established diagnosis, in-patients and day hospital. Patients referred are aged over 65 with suspected Parkinsonism. We see new and review patients, with support of Parkinson’s Disease Nurse Specialists.
Aims
To implement and assess a new model of care for patients newly referred to the Parkinson’s Service, by introducing a telephone appointment prior to first face to face appointment, for patients newly referred to the Parkinson’s Service.
Objectives
To assess whether a telephone consultation prior to attendance:
Is feasible
Fulfils waiting time requirements
Progresses diagnosis
Affects referral and investigation process
Is acceptable to patients
Methods
With the support of the appointments team, initially all new patients were appointed a 30-minute telephone appointment and subsequent 45-minute face to face appointment aiming within 2 weeks of the first telephone call. Telephone appointments were carried out by a Consultant Geriatrician or speciality trainee and all face-to-face appointments carried out by the same Consultant Geriatrician, who specialises in movement disorders. At the face to face appointment, patients were asked to comment on the benefit of the telephone appointment prior to attending in person. Quality improvement methodology was adopted and the PDSA (plan, do, study, act) cycle reviewed on a monthly basis. On subsequent cycles the new referral list was triaged by the Consultant and a decision made as to whether an initial telephone appointment would be helpful. After 3 months, data was collected from the electronic patient records using clinic letters and referral letters of all new patients referred to the Parkinson’s Service. Patient comments were categorised by one assessor as ‘positive’ or ‘negative’. Data was collected on an excel spreadsheet and simple data analysis carried out
Results
We reviewed all new patients appointed between 7th July and 21th October 2021, a period of 15 weeks/ 3.5 months
Of 39 new patients, 24 were appointed under the new model of care. (Table 1). 5 patients cancelled their F2F appointment at initial telephone review under the new model, 1 due to bereavement and 4 due to difficulties attending.
Table 1- Consultation type
| Consultation type | Number |
|---|---|
| New referrals | 39 |
| Telephone reviews | 24 (61.5) |
| Telephone and F2F reviews | 19 (48.7%) |
| Telephone reviews only | 5 (12.8%) |
| F2F only | 15 (38.5%) |
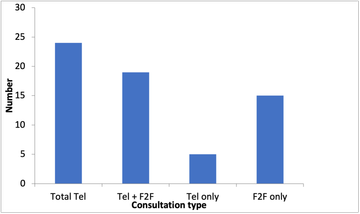
Figure 1- Consultation type
The mean time to review fulfilled waiting time requirements, with most new F2F appointments taking place within target times (12 weeks from referral). (Table 2)
Table 2. Mean time to review
| Time period | Number of weeks (range) |
|---|---|
| Mean time to first telephone review | 10.6 (5-15) |
| Mean time to first F2F review | 12 (5-23) |
| Mean time between first telephone and F2F | 2.2 (1-12) |
The majority of telephone appointments were completed in the new model 21/24 (87.5%). 3/24 (12.5%) did not answer the telephone.
25/32 (78.1%) F2F appointments were completed (83.3%). 2/32 (6.3%) did not attend. 5/24 (20.8%) cancelled at the telephone appointment and 2/32 (6.3%) are not yet seen.
Similar numbers of diagnoses were made at first face to face review both for patients in the new model and with face to face review only. The same diagnosis was often not made at telephone and face to face review. (Table 3) There was a larger range of diagnoses at F2F review (Figures 2 and 3)
Table 3- Percentage of suggested diagnoses made
| Outcome | Number (%) |
|---|---|
| New Diagnosis suggested at first tel appointment | 8/24 (33.3%) |
| New Diagnosis suggested F2F | 25/32 (78.1%) |
| New diagnosis suggested F2F-new model | 12/19 (63.2%) |
| New diagnosis suggested F2F only | 11/15(73.3%) |
| Same diagnosis first telephone and F2F | 3/8 (37.5%) |
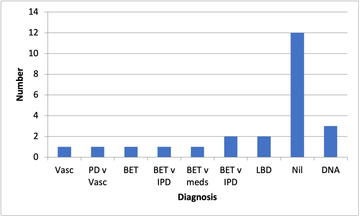
Figure 2-Diagnosis made by telephone
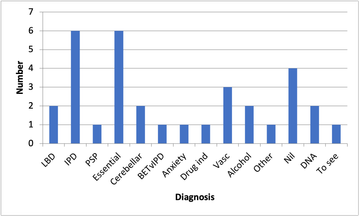
Figure 3- Diagnosis made face to face
In the new model of care a large proportion of people had tests booked at initial telephone appointment (8/19 42%). However, most referrals were made at face-to-face review (10/17 58.8%). (Table 4)
Table 4- Tests and referrals telephone and face to face
| Telephone | % Of All Telephone | %Tel consult prior to F2F | F2F | % All F2F | % Tel+F2F | |
|---|---|---|---|---|---|---|
| Tests ordered | 8 (7 neuro-imaging, 1 bloods) | 8/24 (33%) | 8/19 (42%) | 15 (9 neuro-imaging,1 bloods ,1 MSU) | 15/32 (46.8%) | 10/17 (58.8%) |
| Referrals made | 1 | 1/24 (4.1%) | 1/19 (5.3%) | 15 | 15/37 (40.5%) | 6/17 (35.3%) |
All patients who received a telephone appointment followed by a new F2F appointment had a 30-minute telephone appointment (which was additional to clinic template), plus a 45-minute face to face review appointment. New patients with face to face only appointments received a 60 minute appointment (within existing template).
All patients who had a prior telephone appointment were asked at their face-to-face appointment to comment on the benefit or otherwise of having a preceding telephone appointment. (Table 5, figure 4)
Table 5- Patient views on model of care
| Response | Number (n=19) |
|---|---|
| Positive | 10 (52.6%) |
| Negative | 2 (10.5%) |
| Did not answer telephone | 3 (15.8%) |
| Not yet seen face to face | 2 (10.5%) |
| Feedback not given | 2 (10.5%) |
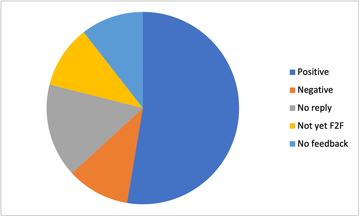
Figure 4- Patient views on model of care
Example comments
'Created relationship'. 'Liked this idea'. 'No rush'. ‘Early re-assurance’.
‘Struggled to pick things up by phone’. ‘Prefer to talk face to face’
Discussion points
This project was carried out in the context of the changing pandemic situation. As such, referral rates and reasons were likely to be affected by this, given the recent different consulting patterns in both primary and secondary care. Our service had been affected due to restrictions of the pandemic with reduced capacity, due to social distancing requirements, and also ‘catching up’ with face-to-face reviews which had been postponed. A speciality trainee in Geriatric Medicine carried out some of the telephone consultations, which may have affected the likelihood of suggesting a diagnosis by telephone. The new model had an impact on the workload of the appointments department. There was also one error in scheduling which accounted for one patient waiting a long time between telephone appointment and face to face review. Due to constraints of time, 2 patients had undergone telephone review but had not yet been seen face to face at the time of analysis. Telephone assessment had been well accommodated during the pandemic and lockdown, however now that people have fewer restrictions, this may have impacted on availability for telephone review.
Conclusions
There are some patients for whom telephone appointments prior to clinic attendance are useful. This is particularly the case for patients who have difficulty attending for physical/practical reasons This model of care allowed us to fulfil waiting time requirements and the time frame between initial telephone contact and face to face review was close to our target. We were less likely to make a diagnosis by telephone than in person. However, we were able to order earlier neuroimaging, in many cases, from making a telephone call first. Referral to other colleagues and departments was predominantly done after a face-to-face assessment. The model of care was predominantly well received by patients, with positive comments for the most part. An issue has been highlighted, however, for those with hearing difficulties communicating by telephone. The model consumes more consulting time than seeing patients directly face to face and there are complexities of scheduling. Therefore, we anticipate continuing to screen referrals prior to appointment, and using this hybrid model of telephone appointment followed by face-to-face review, for a select group of newly referred patients.
References
- Patient and Carer perspectives of Telephone Parkinson’s clinic during the covid pandemic Grounds, M; Marrinan, S;Renton, J. Liberton Hospital, NHS Lothian, Neurology Academy, PD Masterclass online, March 2021
- https://www.gov.scot/publications/supporting-elective-care-clinical-prioritisation-framework/ (accessed 25th Oct 2021)
More Parkinson's Academy Digital health solutions Projects

'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.