How can we address complexity, frailty and multimorbidity in Parkinson's?
Event reportsOur Parkinson's Cutting Edge Science conference took place on 21st June 2023 at Birmingham Conference and Events Centre and was chaired by Prof Emily Henderson.
You can read an overview of the entire event here.
This write up is one of a series covering each session in detail for those who were unable to attend, or want to reflect on what they heard.
The event was sponsored by Bial Pharma. The sponsor had no input into the educational content of the meeting.
Dr Emma Tenison has been researching complexity, frailty and multimorbidity in Parkinson's for the past several years, and began addressing the topic by discussing what we mean by 'clinical complexity'. Noting that multimorbidity, healthcare resource use and psychosocial factors may all impact the complexity of a patients' clinical needs (Schaik et al 2012), Emma shared that dimensions of clinical complexity can include physical, mental and social health and care needs, demographics and social determinants.
Using a figure taken from her 2020 paper (Tenison & Henderson 2020), Emma demonstrated the complex situation that can be caused by a minor event and the issues with clear research findings within this population of people who are often underrepresented in research cohorts (figure 1).

Figure 1: 'The impact of multimorbidity and frailty in Parkinson's disease' taken from Tenison & Henderson 2020
Emma outlined the PRIME study, and its three elements - an epidemiological study, a cross-sectional study (Tenison 2022) and a randomised controlled trial (RCT) (Lithander 2023). The PRIME Parkinson (Proactive and Integrated Management and Empowerment in Parkinson’s Disease) study, initially proposed in 2020, presents a new model of care which is designed to manage problems proactively, deliver integrated, multidisciplinary care, and empower patients and their carers (Tenison 2020).

The epidemiological study sought to describe rates of hospital admission over time and by region, and to determine risks and predictors for unplanned admissions. Emma shared the results of the study, explaining that she has been able to striate the Parkinson's population by age, multimorbidity and likelihood of hospital admission. This potentially opens opportunities for targeted clinical interactions and discussions around preferences and wishes for hospital attendance.
Emma noted that the epidemiological data was able to inform the cross-sectional study, considering the needs of patients with Parkinsonism and their caregivers and tailoring recruitment to gather usually under-represented groups experiencing frailty, complexity or multimorbidity (Tenison et al, protocol for PRIME-UK). Methods included high levels of telephone calls to support recruitment, and the final sample of 477 people with Parkinson's who had been diagnosed for between less than 2 and more than 20 years, appeared to be more representative in comparison to two other similar studies (CPRD and PRISM: Tolosa 2021), .
Emma, within this representative sample, honed in on the aspects of the study pertaining to frailty, sarcopenia (established using screening tool SARC-F), disability and multimorbidity (referring to two or more conditions) and showed the results in a series of Venn diagrams (e.g. figure 2).
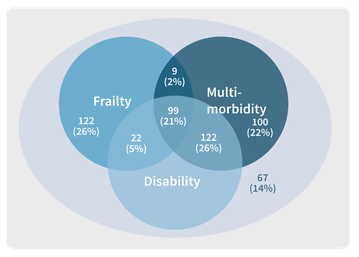
Figure 2: On of several Venn diagrams Emma shared. This one depicts commonality and interrelationship of frailty, multimorbidity and disability in people with Parkinson's from PRIME-UK's cross-sectional study
Her findings included that: those with frailty commonly had either disability or multimorbidity as well, over a quarter of people had coexisting frailty and sarcopenia and those with sarcopenia appeared to have a common progression to pre-frailty then frailty compared to those without sarcopenia.
Emma closed by discussing the protocol for the next phase of the trial, the RCT, which reached 95% recruitment on 19th June. People from the cross-sectional and epidemiological studies have been recruited into this trial, which will test whether a novel model of care can improve health and disease-related metrics whilst being more cost-effective than current forms of care. This will include measuring whether the new model improves goal attainment and decreases hospital admissions.
Questions from the floor
When asked if any specific comorbidities seem to be worse predictors of admission, Emma said that she had not looked at specific comorbidities although there is scope to do so, but that she had looked at causes of admissions.
Another question posted was around whether ethnic background had been taken into consideration; Emma explained that ethnicity was not looked at specifically in this study.
A question about whether, through the risk stratification, there has been an individualised prediction model developed around reducing risk of hospitalisation, Emma confirmed that this has been developed but not yet validated. She also noted that, as well as clinical validation, research into the usefulness of this data would also need to be carried out. For example, would people with Parkinson's find this helpful, or could it potentially induce anxiety?
The recruitment was queried; Emma explained that recruitment was from inpatients to a general hospital (Royal United Hospital, Bath). It was noted by an audience member that some people with Parkinson's are supported more in old age psychiatry than medicine for the elderly and Emma explained that recruitment was across various departments within the hospital to capture the most representative sample within that locality.

Related articles
'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.


