Obesity and neurology: why it's time to address the growing problem
Knowledge
Healthcare thinktank the Kings Fund have produced a new publication assessing the impact of obesity on the health of the nation, and calling for a whole-system approach to tackling the growing problem.
Their findings have significance for neurology, with causal links between obesity and neurological disorders becoming clearer. Additional data examining comorbidities like obesity and socioeconomic status amongst those living with a neurological condition suggests that this is a complex issue, undoubtedly impacting health outcomes, NHS services, financial budgets, and the quality of people's lives.
Tackling obesity on a national scale
The briefing, 'Tackling obesity: the role of the NHS in a whole-system approach' highlights a number of key findings, including a 17% rise in obesity-related hospital admissions in 2019/20 compared the the previous year translating to escalated costs for the NHS, and placing obesity-related admissions at over 1 million in a single year. The Kings Fund also noted that differences in obesity rates translate to worse health outcomes for those in deprived areas, contributing to increased health inequalities.
Whilst highlighting that a whole-system approach is needed, the briefing also suggests that the NHS itself could be doing more to tackle the problem, including targeting services in communities most in need, and using local insights to gather this data. They also call for increased training around nutrition and diet, incentivised referrals to specialist programmes, and more intensive clinical interventions such as surgery.
Obesity in neurology
Whilst obesity itself causes adverse health outcomes, as a comorbidity to a neurological condition it can impact the progression of that condition, or cause additional complexities in its management.
Bhat, 2019
Obesity has been found to increase the likelihood of developing a neurological condition, with research in 2017 outlining the neurological consequences of obesity in the brain and across the body's nervous systems. Some of the issues highlighted by O'Brien included cognitive problems such as mild cognitive impairment, imbalances in the sympathetic-parasympathetic activity of the autonomic nervous system (ANS) and peripheral polyneuropathy (O'Brien, 2017).
A 2017 review of obesity and neurological disorders (published in 2019) of obesity and neurological disorders states that both Parkinson's and Alzheimer's could be initiated through metabolic changes resulting from central nervous system damage - directly caused by obesity (Bhat, 2019).
Further to this, a healthy, varied and unprocessed approach to nutrition, particularly as part of a healthy lifestyle, can have a positive impact on how someone experiences their condition and how they feel in themselves more generally.
Bhat 2019
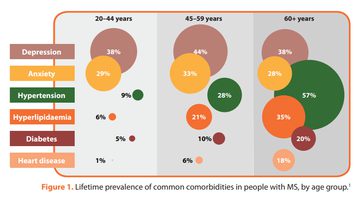
The 'time is brain' initiative in MS has a specific resource for healthcare professionals entitled 'why manage comorbidities in MS?' One of the resources to accompany the key international report, 'Brain health: time matters in multiple sclerosis', it outlines how managing comorbidities and addressing lifestyle-related factors could lead to improved condition management, better quality of life, and slower disease progression.
The initiative, led by experts around the globe introduces the resource on comorbidities:
'MS Brain Health: Time Matters'
From 'MS Brain Health: time matters' 2015, resource 'Why manage comorbidities in MS?' p1
The resource brings together evidence around comorbidity management, and shares positive steps for healthcare professionals to encourage and for people with MS to take, to manage comorbidities such as obesity through positive lifestyle choices.
From 'MS Brain Health: time matters' 2015, resource 'Why manage comorbidities in MS?' p2
From 'MS Brain Health: time matters' 2015, resource 'Why manage comorbidities in MS?' p2
Obesity, social determinants of health and MS
A recent abstract submitted to ECTRIMS 2021 from the Living well with MS workstream, part of Raising the bar for MS, looked at comorbidities and social determinants of health in relation to hospital admissions for people with MS. The abstract, 'Wellbeing gap: one-size MS service does not fit all' made an initial analysis of Hospital Episode Statistics (HES) data to explore emergency hospitalisation in people with MS, and comorbidities that are/may be associated with lifestyle factors, linking to deprivation and socioeconomic status.
The abstract noted that obesity is amongst the top 15 reasons for non-elective admissions amongst people with MS during the financial year of 2020, and that costs for comorbidities such as obesity are higher amongst people with MS than amongst the general populace. The abstract also noted that the wellbeing gap appears higher for deprivation-related comorbidities, confirming the understanding that socioeconomic status is a key determinant of health outcomes.
Dr Agne Straukiene, consultant neurologist and lead of the Living well with MS workstream responsible for the abstract submission said:
References
Bhat ZF, Morton JD, Mason S, Bekhit AEA, Bhat HF. Obesity and neurological disorders: Dietary perspective of a global menace. Crit Rev Food Sci Nutr. 2019;59(8):1294-1310. doi: 10.1080/10408398.2017.1404442 . Epub 2017 Dec 19. PMID: 29257910.
Straukiene A, Chico D, McGowan C, Pomeroy I, Ross R, Fisniku L, Peel C, Berry G, Thomas S, ;'Wellbeing gap: one-size MS service does not fit all', ECTRIMS abstract (submitted for October, 2021.)
O'Brien PD, Hinder LM, Callaghan BC, Feldman EL, 'Neurological consequences of obesity', Lancet Neurology, Review, Vol 16 Is 6, P465-477, JUNE 01, 2017, doi: 10.1016/S1474-4422(17)30084-4
Related articles
Uniquely practical education, producing specialist clinical leaders transforming local healthcare
Neurology Academy is an innovative educational provider for healthcare professionals including consultants, specialist nurses, pharmacists, therapists and other allied health professionals. Our courses are developed by practicing specialists who combine their experience and expertise into case-based learning designed to create specialists in their field with confidence in effecting change.


