Before you watch this webinar
Enhancing your learning experience begins with understanding you better. Collecting data enables us to tailor our educational content specifically for our audience. Discover more about how we handle your information in our Privacy Policy.
Event
Pregnancy and MS: How early should our discussions start, what should be covered and by who and how is this varying around the country
Our sponsor

Case Study:
A 32-year old woman with rapidly evolving severe MS, previously treated with natalizumab for 4 years, but switched to fingolimod 3 years ago when her JCV index went above 1.5. She is now planning to start a family. She has requested going back on natalizumab for her pregnancy. What would you advise?
Objective:
This webinar will discuss how to manage MS DMTs during pregnancy and the management of more active MS during pregnancy. Including some discussion and examples of joint working across MS and Maternity teams.
Sarah White presentation slides
Lucy Lyons presentation slides
Dr Karen Chung presentation slides
Summary
Chair and consultant neurologist Azza Ismail began by setting out the core areas of discussion featured in the webinar, including:
Pre-conception counselling
Management of active MS
Disease-modifying treatments during pregnancy
Establish collaborative working across MS and maternity services
Treatment options for women considering pregnancy
Dr Karen Chung began the first session by remarking on the huge change in family planning options for people with MS over the past 30 years, and the opportunity to support women with MS particularly in this phase of life.
She outlined elements affecting decision-making, including comorbidities, lifestyle and commitments, mode of administration and risk aversion as being relevant to anyone when considering a disease-modifying treatment (DMT). She then added family planning into this, including age and fertility, which can be a challenging discussion to have.
Karen noted that, because clinical trials cannot be run on pregnant women, understanding is based on real-world data and so therefore the best data we have is on those DMTs which have been in use for the longest period which have more than 1,000 examples of use in pregnancy (table 1).
| Continuous therapy | Induction therapy |
|---|---|
| Injectables: interferons and GA | Cladribine |
| Natalizumab | Alemtuzumab |
Table 1: Karen's simplified overview of therapy options during pregnancy
Continuous therapy refers to a treatment given before pregnancy, continuing into the pregnancy and in the postpartum period. Best suited for lower-activity patients.
Increasing confidence is being found in induction therapies for those with higher disease activity. In these cases, Karen suggests interval dosing until around 32 weeks of pregnancy, then ceasing to avoid haematological problems in the newborn.
She went on to use a case study to demonstrate this treatment management in a real life example and encouraged professionals to both utilise the MS pregnancy consensus guidance and to signpost patients towards it, where they are engaged and wish to be more informed.
Pre-conception counselling
Advanced nurse practitioner Lucy Lyons then spoke on the importance of pre-conception counselling, its inclusion in clinical practice and how she established a pregnancy pathway locally.
She outlined the patient survey conducted around family planning which reinforced her own thoughts on a gap in care, and shared personal stories from some of those patients.
In discussing clinical pathway development, Lucy shared the importance of noting triggers for symptom escalations or difficulties in any clinical pathway and to map a pathway for those who have a positive experience of pregnancy without exacerbation of MS symptoms, and also of someone who experience difficulties during pregnancy relating to their MS.
Lucy outlines the importance of having full and transparent discussions between obstetrics teams and women with MS about their monitoring and care, birth and medication planning and preparing for alternative scenarios, all of which should be well documented.
Communication across all care teams, particularly across consultants and teams within MS and obstetrics was highlighted as essential, and Lucy noted the use of shared electronic records in her area to assist in this.
Lucy was also clear about ensuring good, practical and consistent information for people with MS before and during their pregnancy, from remembering to ask about family planning needs in clinic and referring to pre-conception counselling where relevant (table 2), to providing the best possible information to people thereafter. She noted that often, women considering pregnancy may also be newly diagnosed and therefore navigating information around their MS itself and the future impact on family life as well.
| Pre-conception counselling topics to cover | |
|---|---|
| Disease-modifying treatments (DMTs) | Vaccines |
| Symptomatic treatment | Mode of delivery |
| Vitamin D | Post-partum logistics and support inc sleep deprivation, new routine, breastfeeding, etc. |
| Smoking cessation |
Table 2: Lucy shares the topics she covers at a pre-conception counselling session
A combined Maternal Medicine and MS service
Senior MS Nurse Specialist Sarah White presented on the combined Maternal Medicine and MS service that was established a few years ago within St George's University Hospitals, after a lady with MS reported having felt unprepared during her own pregnancy (fig 1).
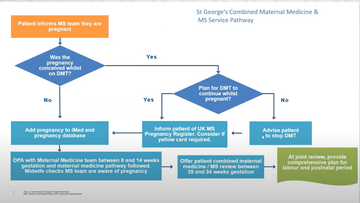
Figure 1: A condensed version of the combined Maternal Medicine and MS service pathway shared by Sarah during her session.
Sarah outlined key elements of discussion which takes place at the joint review with both maternal medicine and MS representatives present, often the MS nurse and midwife (table 3).
| Joint maternal medicine and MS meeting topics | |
|---|---|
| Birth plan | Post-partum support plan |
| Post-partum relapse risk | Symptom management |
| Breastfeeding | DMT plan |
Table 3: Sarah shares the topics covered at a joint maternal medicine and MS meeting with the pregnant woman with MS
Sarah provided a range of practical advice and tips to support new mothers, from arm slings to aid with fatigue in breastfeeding, to modified prams, social groups and medication support. She also highlighted the need to be vigilant about postpartum depression and domestic abuse, both of which have increased rates in the first year postpartum (Kornfeld 2012), and shared the latest MBRRACE-UK figures which stated that 13% of all women who died within the first year of a pregnancy died as a result of a mental health condition.
She shared the importance of collaborative working and the benefit that both midwives and MS nurses have found in expanding knowledge and understanding through this joint working.
Sarah closed her session with a number of ideas for putting this form of collaborative working into practice:
Ask patient for details of their named midwife for sharing information
Arrange to review the patient yourself between 28 and 34 weeks of pregnancy
Find out contact details for local support services like feeding teams, and safeguarding of mental health midwives or health visitors
Find out about Birth Reflections services
Increase personal awareness of risks around domestic abuse and mental health
Familiarise yourself with the MS pregnancy joint consensus guidance
Consider setting up a joint clinic with a midwife
The session ended with speakers responding to a variety of questions, from minute 49.29 onwards.
More information
All speakers encouraged the use of:
the UK MS register, accessed at www.ukmsregister.org/pregnancy which will help to provide a great deal more data on MS medication use during pregnancy as more people with MS sign up for it.
Additional references made included:
MBRRACE-UK: Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK, accessed: www.npeu.ox.ac.uk/mbrrace-uk
Kornfeld BM et al, 'Postpartum Depression and Intimate Partner Violence in Urban Mothers: Co-Occurrence and Child Healthcare Utilization', Journal of Paediatrics, vol161, is2, p348-353.E2, Aug 01, 2012, DOI: doi.org/10.1016/j.jpeds.2012.01.047
Podcast
Our Multiple Sclerosis webinars are available on SoundCloud:
soundcloud.com/neurologyacademy
Our sponsor

Chair
 Dr Azza Ismail
Dr Azza IsmailConsultant neurologist, Sheffield teaching hospitals NHS foundation trust
Speakers
 Dr Karen Chung
Dr Karen ChungConsultant neurologist, University College London Hospitals NHS Foundation Trust
 Lucy Lyons
Lucy LyonsAdvanced Nurse Practioner, The National Hospital for Neurology and Neurosurgery (NHNN)
 Sarah White
Sarah WhiteLead MS specialist nurse, St. George’s University Hospitals NHS Foundation Trust
Encouraging excellence, developing leaders, inspiring change
MS Academy was established in 2016 and in that time has accomplished a huge amount with exciting feedback demonstrating delegates feel inspired and energised along their personal and service development journeys. The various different levels of specialist MS training we offer are dedicated to case-based learning and practical application of cutting edge research.