A retrospective analysis of clinical outcomes and bone protection prescribing in patients with parkinsonism and neck of femur fractures
Having undertaken clinical attachments in Orthogeriatrics throughout my SpR training, I have looked after a number of patients with Parkinson’s Disease (PD) who have been admitted with hip fractures. After attending the Parkinson’s Masterclass earlier this year, I decided to undertake a quality improvement project (QIP) on bone protection and clinical outcomes in this cohort. I modelled the project on a study published by Walker et al,[i] which used local data from the National Hip Fracture Database (NHFD), and expanded the project design to incorporate more data on bone protection.
Background
In the UK, approximately 536,000 new fragility fractures occur each year, of which 79,000 are hip fractures which cost the NHS and social care approximately £1 billion per year. Despite 30-day morality rates dropping to 6.2% in the 2016 NHFD, up to a third of patients still die within a year. [ii], [iii] It is reported that PD patients suffer worse outcomes following hip fracture, including length of stay and increased dependency.1
Falls are common in PD and often multifactorial, relating to such factors as postural instability, motor fluctuations, medication, postural hypotension and cognitive impairment. Meanwhile, PD is a major independent risk factor for osteoporosis and fragility fractures.[iv], [v] It is estimated that osteoporosis affects as many as 91% of female patients and 61% of male patients.[vi] PD patients are twice as likely to suffer an osteoporotic fracture compared to non-PD counterparts, and thrice as likely to suffer a hip fracture.[vii], [viii] In fact, the median time from diagnosis to hip fracture is 4 years, with most patients suffering a fracture in mild to moderate stages of disease.7
Despite a recent update to the NICE guidelines for PD in 2017,[ix] there remains a lack of national guidance on managing bone health in PD. More generic recommendations from NICE Osteoporosis Guidance advocate using FRAX or Q-Fracture scoring tools to identify patients at risk of fragility fracture in the general population.[x] A paper published by Lyell et al suggests that PD patients over 75 years of age with Q-Fracture scores of ≥20% for major osteoporotic fractures and/or ≥5% for hip fracture should be considered for bone protection without the need for a DEXA scan.7
Aim
To review bone protection management and clinical outcomes for PD patients admitted with hip fractures in our local hospitals (Heart of England NHS Foundation Trust).
Study design and method
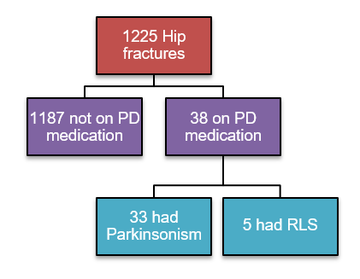
Data was collectively retrospectively from the trust’s NHFD from 1st April 2014 until 31st December 2016, covering a total of 32 months and 1,225 hip fractures. Comorbidity is not logged on the NHFD so, to identify PD patients, our IT department generated a list of all patients admitted to our Electronic Prescribing system during this timeframe who had been prescribed recognised Parkinson’s medication. These hospital numbers were then matched to those listed on our local NHFD records, giving a total of 38 patients. Patient records were then reviewed to confirm a genuine diagnosis of Parkinsonism in 33 patients, representing 2.7% of all hip fracture admissions.
Subsequently, clinic letters, discharge letters and scanned admissions notes were reviewed in detail to elicit data on: previous falls, previous fragility fractures and type of Parkinsonism. Using the NHFD, data was obtained on: pre-admission osteoporosis treatment, pre-admission residence, delays to theatre, length of stay (LoS), post-discharge osteoporosis treatment and post-discharge residence. Patient letters were reviewed 6 months post-discharge to ensure those pending clinic follow-up or DEXA scan results ultimately had bone protection prescribed. Theoretical pre-admission Q-Fracture scores were also calculated for all patients.
Results
All 33 patients with Parkinsonism were included in the study and are hereafter referred to as PD patients for simplicity. 27 patients (82%) had a diagnosis of Idiopathic Parkinson’s Disease, whilst the remainder had Vascular Parkinsonism (2 patients) or an unspecified diagnosis of Parkinsonism (4 patients). Average age was 84 years (range 71-96) compared to 81 years for the non-PD population. 18 patients were male and 15 were female. 24 patients (73%) were under regular follow-up, either with Geriatrics or Neurology. 9 patients were not under regular follow-up which included 4 new diagnoses.
Analysis of pre-admission records established 12 patients (36%) were documented to have a previous fragility fracture and 21 patients (64%) were documented to have falls. 4 patients (12%) were on osteoporosis treatment. Of note, 9 of those with previous fragility fracture were not on osteoporosis treatment. 6 patients (18%) were on Calcium/Vitamin D preparations. Theoretical pre-admission Q-scores were high: average 10 year hip fracture risk was 44%; average 10 year osteoporotic fracture risk was 43%.
13 (39%) of PD patients experienced a delay to theatre of >36 hours whereas only 25% of non-PD patients has such delays. 4 of these delays occurred due to theatre list schedules, 4 were deemed medically unfit, 2 needed medical review or optimisation and 3 were awaiting further orthopaedic investigation. PD patients had a similar average LoS to non-PD patients: 22.6 days (range 6-58) compared to 21.8 days (range 2-153 days). However, median LoS was much higher for PD patients: 21 days compared to 16 days.
6 (13%) PD patients were originally from a nursing home (NH), whereas 13 (39%) were discharged directly to a NH. In comparison, only 113 (9%) of non-PD patients were originally from a NH but 196 (16%) were discharged directly to a NH.
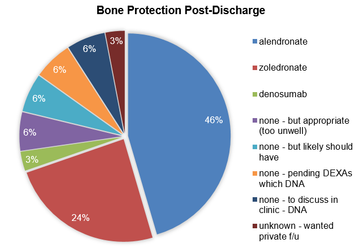
24 PD patients (72%) were on osteoporosis treatment 6-months post-discharge, with an equal male/female distribution. 15 were treated with Alendronate, 8 with Zoledronate, and 1 with Denosumab. All but 2 PD patients were discharged on Calcium/Vitamin D treatment. Of note, 1 patient had primary hyperparathyroidism. 5 patients had DEXA scans requested to facilitate management decisions; 4 were female and 3 of these were in their 80s. In total, 4 patients did not receive bone protection as a consequence of not attending follow up scans or outpatient review. 1 patient wanted private follow-up and had an unknown outcome. After review of the notes, an additional 2 patients (both male) were likely to have been suitable for bone protection but were not treated. 2 patients were unsuitable for bone protection – either too unwell or extremely frail.
Analysis
A significant number of PD patients were documented to have falls (64%) or previous fragility fractures (36%), yet only a minority (12%) were on osteoporosis primary or secondary prevention treatment. Theoretical pre-admission Q-Scores support the conclusion that most of these patients should have been on bone protection prior to admission.
Once admitted, PD patients were more likely to experience a delay to theatre (40% compared to 25%) and had a longer median LoS (21 days vs. 16 days). Admission with a hip fracture conveyed a 3-fold likelihood of discharge to a nursing home for PD patients but only a 2-fold increase for non-PD patients.
Once discharged, bone protection was prescribed in less than 3/4 of cases. Some patients were awaiting follow-up DEXA scans or outpatient clinic appointments which were not attended, whereas more definite decisions could have been made whilst inpatients. DEXA scans were requested in several cases where osteoporosis could be assumed. A pragmatic approach was evident in managing male patients, with a DEXA scan request in only 1 patient.
Discussion and recommendations
This results support the preconception that PD patients have poorer outcomes when admitted with a fractured neck of femur. Bone protection prescribing is suboptimal both pre-admission and on discharge. The QIP data will be presented at a local meeting to increase awareness of these problems.
For outpatients, a non-motor questionnaire could be routinely sent out prior to clinic attendance, highlighting those with falls with a suggestion to then calculate the Q-Fracture score. A clinic pro-forma has been considered but can disrupt the flow of a consultation. A modification to the trust’s NOF admission booklet will be suggested, incorporating a section on PD which references the trust’s PD guidelines, and a prompt to get a specialist review. Furthermore, a streamlined Zoledronate/Denosumab pathway has been made for our medical day hospital which should facilitate discharging these patients on non-oral bone protection when needed.
References
- Walker et al. Hip fractures in people with idiopathic Parkinson’s disease: incidence and outcomes. Mov Dis. 2013; 28: 334–40.
- Clinical guideline for the prevention and treatment of osteoporosis. NOGG. Updated March 2017. https://www.sheffield.ac.uk/NO... (accessed 13.11.2017).
- National Hip Fracture Database 2017. Annual Report. https://nhfd.co.uk/files/2017R... (accessed 13.11.17).
- Van den Bos et al. Parkinson’s disease and osteoporosis Age Ageing. 2013; 42: 156–162.
- Torsney et al. Bone health in Parkinson’s disease: a systematic review and meta-analysis. JNNPsych. 2014; 85:1159–1166.
- Invernizzi et al. Osteoporosis in Parkinson’s disease. Park Rel Dis. 2009; 15: 339–346.
- Lyell et al. Assessment and management of fracture risk in patients with Parkinson’s disease Age Ageing. 2015; 44 (1): 34-41.
- Pouwels et al. Risk of fracture in patients with Parkinson’s disease. Osteo Int. 2013; 24: 2283.
- Parkinson’s Disease In Adults. NICE Guidance. Updated July 2017. (https://www.nice.org.uk/guidan... (accessed 13.11.2017).
- Osteoporosis: assessing the risk of fragility fracture. NICE Guidance. Updated February 2017. https://www.nice.org.uk/guidan... (accessed 13.11.2017).
More Parkinson's Academy Falls & bone health Projects
'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.