Learning Hub on Parkinson’s for health care professionals and patients at East and North Herts NHS Trust
Background
There are approximately around 300 patients with Parkinson disease looked after mostly Neurology team based at Lister,QE11 and Herford County Hospitals. The main part of the PD service is one hospital based, PD nurse. Consultant Geriatrician set up ad hoc weekly PD clinic based at Lister Hospital.
In our project, we perform a questionnaire survey regarding educational needs and opportunities about Parkinson disease for junior doctors and nurses at North and East Hertfordshire Trust.
These survey results were taken from 27 junior doctors and 20 nurses in the Lister Hospital.

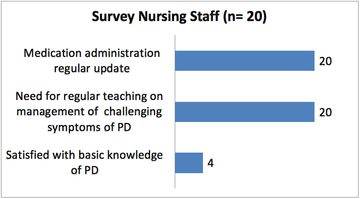
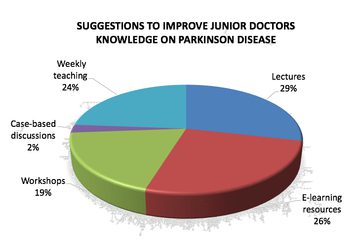
We recognised that while most junior doctors were confident in identifying P.D , Junior doctors were not as confident in prescribing anti-parkinsonian medications, identifying a parkinsonian crisis and managing a parkinsonian crisis. Junior doctors also were not familiar with the referral process for PD within the trust. Nursing staff lack completely in knowledge regarding management of challenging symptoms of PD. 20/20 asked for regular update on medication administration and they were also very keen to learn about basics of PD. When asked for suggestions on how to improve the level of PD related knowledge among junior doctors, the 3 most popular suggestions were: (1) lectures (2) e-learning resources and (3) incorporation of PD educational sessions as part of weekly junior doctor teaching.
Therefore, we proposed the Educational Programme for Junior doctors and Nursing staff:
A. 2 monthly teaching for Juniors doctors in the elderly care as part of departmental mandatory teaching that included:
- PD pathophysiology
- Motor and non- motor symptoms recognition
- Management of challenging symptoms and complications
- Differentials diagnoses
- Local services update
B.1 monthly ward based teaching for nurses and HCA that included:
- Basics of PD
- Challenges in management of symptoms control motor and non-motor
- Medication administration: GET it on time
C. After successful feedback from two groups above we decided to create separate one to one teaching session for patient in the clinic based at Lister Hospital. This is yet to be evaluated.
Outcome measures:
A. Clinician group
- Clinicians should be able to confidently recognise potential Parkinsons’ Disease patients and differentiate appropriately
- Clinicians should be able to understand where to refer potential cases of PD and be aware of local services
- Clinicians should be able to confidently/safely prescribe Parkinsons’ Disease medication (continuation of treatment)
- Clinicians should be able to identify and manage Parkinsonian Emergencies
B. Nursing staff group
- Staff nurse should be able confidently understand the basics of Parkinson disease and challenges associated with the symptoms of Parkinson’s
- Staff nurse should be able to understand where to refer potential cases of PD and be aware of local services
- Staff nurse should be able to confidently/safely administer Parkinsons’ Disease medication
C. Patient group
- Patient should be able confidently understand the basics of Parkinson disease
- Patient should be able to understand where to seek advice and be aware of local services
- Patient should be able to confidently understand how to take medication and recognise side effects
- Patient should be able confidentially to know about the resources available online and/or written
Feedback:
A and B group
Post teaching feedback: 100% satisfaction both groups clinician and nursing staff.
Conclusion:
In our survey, we recognised that the North and East Hertfordshire Trust lacks of structured learning opportunities and training about Parkinson Disease for junior doctors and nurses. We also identified lack of knowledge about local services and system referral. We proposed 2 monthly learning hub for elderly care trainees and monthly ward based teaching for nurses to fill in the gaps.
The programme appears to provide a promising means for empowering junior doctors and nurses to deal with challenges of Parkinson disease.
The next stage of our project is to repeat our survey with the same questionnaire and review our proposed educational programme. Also our ambition is to involve the patient in the clinic for face to face individualised teaching sessions.
More Parkinson's Academy Education Projects
'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.
