Balancing treatment burden and capacity
Event reportsOur seventh Parkinson's Cutting Edge Science conference took place on 19th March 2024 in Birmingham and was chaired by Prof Emily Henderson and Dr Neil Archibald. You can read an overview of the entire event here.
This write up is one of a series covering each session in detail for those who were unable to attend, or want to reflect on what they heard. Read more session write ups here.
Treatment burden, and a person’s ability and willingness to manage it, are directly linked to outcomes in Parkinson’s disease.
Presenting her research at this year’s Cutting Edge Science for Parkinson’s Clinicians conference, held in Birmingham in March, Dr Qian Yue Tan, consultant geriatrician at Portsmouth Hospitals University NHS Trust, stressed the need to balance treatment regimens with each patients' capacity to manage their health.
Defining the problem
Treatment burden is defined as the workload of healthcare and its impact on patient well-being and function, whereas capacity is the ability and willingness to access and utilise the resources needed to address this workload.
Healthcare workload can include taking medications, attending appointments, and adapting to lifestyle changes. All this, said Dr Yeu Tan, has to be balanced with everyday life demands.
“A patient’s ability to manage this workload is influenced by their capacity, which can be affected by many factors, including their physical and mental ability, their social support, and their economic resources,” she said.
All of these factors impact on whether they are in the position to access and utilise services, or enact self-care, to manage their health.
“Any imbalance of the two, either due to high workload or reduced capacity, can lead to poor outcomes, such as poor quality of life, or poor adherence to medications and resources.”
This is particularly important in Parkinson’s, as people are managing multiple motor and non-motor symptoms, and many are living with co-morbidities and frailty. It means that they, and their loved ones, are at risk of experiencing high treatment burden and reduced capacity.
The study
Dr Yeu Tan’s four-part study aimed to explore the experience of treatment burden and capacity in Parkinson's and the impact of multi-morbidity and frailty, as well as identify potentially modifiable risk factors.
First, a systematic review of the existing literature, found the main issues of treatment burden in Parkinson’s related to medications, as well as accessing information and healthcare provision.
This was “not surprising”, Dr Yeu Tan said, considering the complex nature of Parkinson’s treatment, the huge volume of disease education often required at diagnosis, and the lack of co-ordination between healthcare services.
Next, researchers conducted a series of semi-structured interviews with nine people with Parkinson’s and eight caregivers. “Our findings built upon what we found in the systemic review: treatment burden and capacity were really interlinked.” (see fig 1).
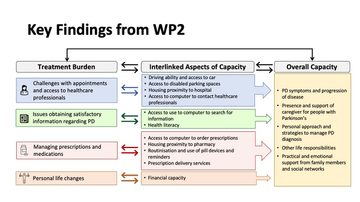
Fig 1: Key findings from semi-structured interviews
The team also conducted a national survey of 160 patients and 30 caregivers. Participants, drawn from clinics with the support of the Parkinson’s UK Take Part Hub and the Research Support Network, completed the Multimorbidity Treatment Burden Questionnaire (MTBQ).
Among the people with Parkinson’s, worsening disease severity, higher number of non-motor symptoms, frailty, and taking medications more than three times a day were all associated with higher workload. Access to transport and technology, proximity to services, and health literacy all impacted on capacity.
There was no association with multimorbidity or the number of medications, but “the qualitative component of our study suggests that it does have an impact,” said Dr Yeu Tan.
For caregivers, caring for someone with memory issues increased treatment burden, and lower scores on the mental health component of the MTBQ were associated with higher caregiver burden. “Caregivers reported that it was adjusting their own lifestyle to look after the person they cared for that was the most difficult,” she added.
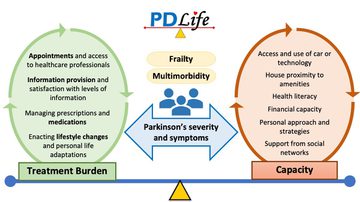
Fig 2: Balancing treatment burden and capacity
The final part of the project was a series of three focus groups with key stakeholders, aimed at developing recommendations on how to reduce burden and enhance capacity.
Participants included three people with Parkinsons, one caregivers, three specialist Parkinson’s clinicians, two community clinical pharmacists, a consultant old age psychiatrist, and a community physiotherapist.
They discussed the need to increase the visibility of Parkinson’s among non-specialist healthcare professionals, through awareness raising and education, improve the availability and organisation of health care services, and enhance communication.
Implications for practice
Said Dr Yeu Tan: “It is tricky, because of the capacity in NHS resources is limited already, but we could think about more flexible structures. Do we need to see everybody every six or 12 months? Some people need more appointments, others could contact services when they feel their symptoms need to be looked at.”
For those who are comfortable with technology, utilising solutions such as remote appointments and symptom monitoring, could also help to reduce the burden associated with attending appointments, members of the focus groups said.
They also spoke about improving HCP/patient communications, highlighting the importance of using plain language, setting realistic expectations of treatment and other interventions, and suggesting a role for “lay summaries” of clinic letters.
Summing up, Dr Yeu Tan said not all treatment burden is avoidable, and not all treatments are burdensome, but it was important to understand the positive effects of managing reduced capacity.
“Perhaps we need to be looking at how do we encourage our patients and their caregivers to increase their self-management strategies,” said Dr Yeu Tan, adding that teams can signpost people to existing sources of capacity-boosting support, such as Parkinson’s UK symptom management advice.
“Early recognition and awareness that lots of our patients may be experiencing treatment burden is the first step. Now we are aware that it exists, we can look at addressing it, perhaps by using the MTBQ in our clinical practice.”
Acknowledging that time constraints may not always allow this approach, she said even identifying and seeking to address “the most difficult” aspect could be helpful for those who are struggling.

This meeting is designed and delivered by the Parkinson’s Academy and sponsored by BIAL Pharma. The sponsor has had no input into the educational content of this meeting.
Related articles
'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.








