Before you watch this webinar
Enhancing your learning experience begins with understanding you better. Collecting data enables us to tailor our educational content specifically for our audience. Discover more about how we handle your information in our Privacy Policy.
Event
Exercise in Parkinson's during COVID-19
Our sponsor

This activity has been supported by sponsorship from and Bial. The sponsor has had no control over the educational content of this activity.
Summary
Introduction
Dr Richard Davenport began by sharing that a number of people living with Parkinson’s have been struggling during this time of lockdown due to inactivity, among other things. He noted that, whilst he intrinsically encourages exercise as a positive thing amongst his patients, he is not personally aware of the evidence base beyond nuances like dance therapy. However, there is a significant evidence base and he welcomed Bas Bloem and Fiona Lindop to share more.
The evidence base for exercise
Prof Bas Bloem began by highlighting the book, ‘Ending Parkinson’s Disease’ and noted that within it is the evidence base that:
- Parkinson’s is the fastest growing neurological disease on the planet, and we think that it is, to an extent, a man-made disease.
- By regularly engaging in exercise and adhering to particular nutrition, we can reduce the likelihood of developing Parkinson’s.
All of us tend to be inactive but for someone with Parkinson’s this can be harder due to physical difficulties with balance, gait and freezing, cognitive problems like depression and apathy, and even general physical difficulties like fatigue.
- As Parkinson’s progresses, the level of inactivity increases (vanNimwegen, 2011)
- The adverse effects of inactivity include cardiovascular disease, osteoporosis, insomnia, cognitive decline, depression, constipation, and all lead to early mortality. All of these are risk factors when you have Parkinson’s, so if you are both inactive and have Parkinson’s your risk of early mortality are higher.
A paper in Nature Neurology (Speelman, 2011) outlines the reasons why people with Parkinson’s ought to exercise. To sum it up, Bas noted:
- Anyone who exercises has better bone and mental health and lower risk of cognitive decline
- Specific benefits for those with Parkinson’s are that exercise suppresses motor symptoms much as a drug does, as well as helping address some non-motor symptoms like sleep, depression, cognitive difficulties and constipation.
Can we prescribe exercise as we would a drug? We need to consider the risks too; falling and stumbling for example; and how we customise it to personal preferences and needs.
- The first study to examine the dosing effects of exercise (Moore, 2013)
- Evaluated the impact of both with moderate and high intensity exercise, and with different time amounts, or ‘time doses’ (fig 1)
- Used the Unified Parkinson’s Rating Scale to measure overall symptoms and progression.
- Found that, over time, the high intensity group stabilised their symptoms, moderate intensity helped stabilise motor symptoms, control worsened over time (fig 2).
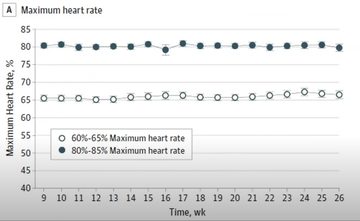
Figure 1: Table showing the two groups of people asked to exercise moderately or strenuously
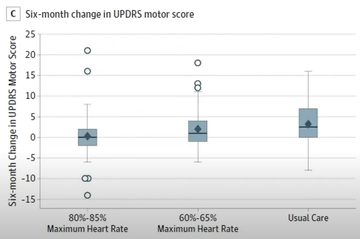
Figure 2: Table showing the outcomes where the y axis is the unified Parkinson’s rating scale and the x axis is the three groups – high intensity (left), moderate intensity (centre) and control group (right)
- V-TIME study looked at multimodal stimulation of the brain using a 3-D environment through virtual reality alongside a treadmill.
- The results found that treadmill running alone reduced the likelihood of falls in people with Parkinson’s or mild cognitive impairment (MCI)
- However, using a treadmill alongside the virtual reality input reduced falls more significantly (fig 3).
- The downside of the study was the need for people to travel to the hospital three times weekly to access the equipment, which was a motivational barrier for many.
- Other barriers included low expectations of outcomes, a lack of personal time, and a fear of falling during exercise.
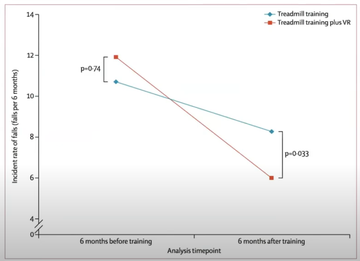
Figure 3: V-TIME study findings of falls reductions in those using a treadmill versus those using a treadmill and virtual reality input
The learning from the V-TIME study was used to develop the Park-in-Shape (van der Kolk, 2015)
- Based on learning that someone with Parkinson’s who could not walk due to freezing may still cycle without difficulty (interview with Bloem in Road.cc; Stamelou, 2011), the study put static exercise bicycles into people’s homes, removing the fear of falling, the barrier of physically going to the hospital to exercise.
- There were rewards built into the process supported by family members, as well as gaming elements (termed ‘exergaming’) such as ‘Pacman’ where the individual had to cycle faster to move the icon around the screen and ‘kill the monsters.
Another study (van der Kolk, 2019) compared this group of Parkinson’s using ‘exergaming’ for their activity with those with Parkinson’s who were stretching for their form of activity, using the rewards app in both groups (fig 4). - The study found that, when sufficiently motivated, people with Parkinson’s can exercise regularly at home.
- It also found that the aerobic group had a stabilisation of their motor symptoms.
Figure 4: People with Parkinson’s counteracting sedentarism through aerobic exercise or stretching
Finally, Bas presented a paper which is currently under submission to the Lancet Neurology looking at brain MRI in the same groups as the previous study – the aerobic versus stretching group. The content is currently embargoed but the brain scans found brain-related benefits for those within the aerobic group which are incredibly positive.
Presentation slides
Fiona's slides
Resources
- Book ‘Ending Parkinson’s disease’: endingpd.org
- van Nimwegen et al. Physical inactivity in Parkinson’s disease. J Neurol. 2011
- Speelman et al. How might physical activity benefit patients with Parkinson disease?. Nat Rev Neurol. 2011
- Schenkman M, Moore CG, Kohrt WM, et al. Effect of High-Intensity Treadmill Exercise on Motor Symptoms in Patients With De Novo Parkinson Disease: A Phase 2 Randomized Clinical Trial. JAMA Neurol. 2018
- Mirelman A, Rochester L, Maidan I, et al. Addition of a non-immersive virtual reality component to treadmill training to reduce fall risk in older adults (V-TIME): a randomised controlled trial. Lancet. 2016
- van der Kolk, N.M., Overeem, S., de Vries, N.M. et al. Design of the Park-in-Shape study: a phase II double blind randomized controlled trial evaluating the effects of exercise on motor and non-motor symptoms in Parkinson’s disease. BMC Neurol 15, 56. 2015
- Snijders AH, Bloem BR. Images in clinical medicine. Cycling for freezing of gait. N Engl J Med. 2010
- van der Kolk NM, de Vries NM, Penko AL, et al. A remotely supervised home-based aerobic exercise programme is feasible for patients with Parkinson’s disease: results of a small randomised feasibility trial. J Neurol Neurosurg Psychiatry. 2018
- van der Kolk NM, de Vries NM, et al. Effectiveness of home-based and remotely supervised aerobic exercise in Parkinson’s disease: a double-blind, randomised controlled trial. The Lancet. 2019
- Wallén et al. Levels and Patterns of Physical Activity and Sedentary Behavior in Elderly People With Mild to Moderate Parkinson Disease. Physical Therapy. 2015
- Bouça‐Machado et al. Physical Activity, Exercise, and Physiotherapy in Parkinson’s Disease: Defining the Concepts. Movement Disorders Clinical Practice. 2019
- De Biase et al. The COVID-19 Rehabilitation Pandemic. Age and Ageing. 29 May 2020
- Afshari M, Yang A, Bega D. Motivators & barriers to exercise in Parkinson’s disease. J Parkinson’s Dis. 2017
- Nilsson MH, Iwarsson S et al. Barriers & facilitators for participation in people with Parkinson’s Disease. J Parkinson’s Dis. 2015
- Lee, JH; Choi, M et al. Impacts of an Exercise Program and Motivational Telephone Counseling on Health-Related Quality of Life in People With Parkinson’s Disease. Rehab nursing. 2019
- Hermanns M, Haas B et al. Engaging older adults with Parkinson’s disease in physical activity using technology:a feasibility study. Gerontol Geriatr Med. 2019
- Lai, B; Bond, K et al. Exploring the uptake and implementation of tele-monitored home-exercise programmes in adults with Parkinson’s disease: A mixed-methods pilot study. J Telemedicine and Telecare. 2018
- van Eijkeren FJ, Reijmers RS, Kleinveld MJ, Minten A, Bruggen JP, Bloem BR. Nordic walking improves mobility in Parkinson’s disease. Mov Disord. 2008
Exercise links
- Power for Parkinson’s: 10-minute videos
- Reach Your Peak: 2 weeks free, personalised, daily exercises
- Parkinson’s UK: YouTube exercise classes (live on Facebook)
- Parkinson’s Wellness Recovery (PWR): free exercises
- Dance: Spread Your Wings – Dancing through Parkinson’s
- Parkinson’s Life: 5 Parkinson’s exercise classes for keeping fit in lockdown
- European Parkinson’s Disease Association (EPDA): ExerciseCast programme
- Parkinson’s Foundation: Fitness Fridays
Parkinson’s UK links
- Advice booklet: Parkinson’s and Coronavirus: your questions answered
- Advice for patients on telephone & video appointments
- Resources for professionals relating to COVID-19
- Nordic walking and Parkinson’s
Exercise apps
- PD Warrior: free app with 10 free exercises
- Clock Yourself App
- Podcast: The Parkinson’s Podcast – How to exercise better with Parkinson’s
Nordic walking
→ Nordic walking for Parkinson’s: warm up exercises (15 mins video)
Our Parkinson’s COVID-19 webinars are available on SoundCloud:
soundcloud.com/neurologyacademy
Our sponsor

This activity has been supported by sponsorship from and Bial. The sponsor has had no control over the educational content of this activity.
'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.


