Before you watch this webinar
Enhancing your learning experience begins with understanding you better. Collecting data enables us to tailor our educational content specifically for our audience. Discover more about how we handle your information in our Privacy Policy.
Event
Pain management in Parkinson's
Our sponsor

Join Patsy Cotton and Robin Fackrell as they discuss Parkinson’s related pain and its treatment. This discussion will include case studies and communication strategies employed in how to best engage with your patients on this matter.
What is pain in Parkinson's? How do we establish if the pain is Parkinson's related or not? What are the treatment options available?
CPD accreditation
Pain management in Parkinson's has been approved by the Federation of the Royal Colleges of Physicians of the United Kingdom for 1 category 1 (external) CPD credit(s.
Please note CPD Federation approval does not include satellite symposia sessions.
Presentation slides - Patsy Cotton
Presentation slides - Dr Robin Fackrell
Summary
Patsy Cotton, Parkinson's nurse specialist, begins this webinar by posing a range of questions relating to pain and people with Parkinson's, chiefly asking 'do people with Parkinson's really experience pain, and is it reported amongst 50% of people living with the condition?
She goes on to list a whole range of different types of pain that patients have reported, both in terms of its location, from muskuloskeletal, to abdominal, whether its widespread or focused in one place such as the bladder or mouth, and the sensation it gives, from tingling to burning, aching to shooting (Chaudhuri 2015).
End stage Parkinson's is associated with some pain, particularly with withdrawal of medicine - but Patsy noted a study stating that 85% of people with Parkinson's at the end of life experience pain (Higginson 2012). Patsy suggested that this is concerning and raises questions around whether people are getting the right medication management towards the end of their lives.
Patsy shared that pain is likely a non-motor symptom in its own right, though one that is perhaps not addressed properly or consistently, and that the presence of pain as a symptom may pre-date diagnosis.
Literature reviews find a huge variation in prevalence of pain in Parkinson's from 45-85% and it can be difficult to know whether pain that someone with Parkinson's is experiencing is related to their Parkinson's or to some other health difficulty.
Patsy then took the audience through a case study, or a current patient she has who manifested with pain as a primary symptom, and a few other irregularities such as discoordination, for a year or so prior to diagnosis. This patient was a fit and active ex-GP who wrote his story for her to share and who closed by saying:
'I was aware of the typical Parkinson's symptoms but never was aware that limb pain could be one. None of my GP colleagues were either.'
Dr Robin Fackrell then opened his section of the talk with the question, 'what is pain?'.
'Pain means different things to different people, and it's always a personal experience influenced by your biology, your psychology - with people having different 'pain thresholds', and what it is you're doing; social factors and emotion play a huge part in how people experience pain.'
Robin clarified that pain and nociception are different things, and that pain should not be assumed where there is a stimulation of nociceptors. He also highlighted the importance of respecting people's own interpretations of their pain, being clear that how people respond to pain and learn their pain and responses to it is uniquely shaped by their individual lives.
Whilst pain serves an adaptive role, Robin was clear that - as with many non-motor symptoms - it can have an adverse affect on social and emotional experiences and greatly impact quality of life. He was also keen to point out that whether someone can articulate or communicate their pain or not does not impact whether they are experiencing it.
Robin reiterated Patsy's case study; he noted that the literature on pain is reasonably limited, only garnering interest in the last decade or so, but that there is evidence that pain can often be pre-motor and pre-diagnosis (Tai 2020).
Dopamine is closely involved in people's appreciation of pain due to the thalamic, basal ganglia and cortical areas of the brain, as well as the limbic system, all connected with pain, adding to both the complexity of pain in general, and of that experienced by people with Parkinson's specifically.
Rather than digging into the neurochemistry of pain, Robin provided a simplified version of the pain process:
pain sensitivity stimulation of nociceptors
impulses sent via the dorsal horn in the spinal cord via peripheral nervous system
message travels to the central nervous system - and there are ascending and descending pathways.
Robin then looked at this process in the context of why those with Parkinson's may experience pain. Pain is more likely to be experienced by female Parkinson's patients (Martinez-Martins 2012) and those with early onset Parkinson's, whilst those who experience pain are likely to continue to go on and experience more, for many reasons.
Robin noted that things like postural change, motor change and dystonia can all cause pain, whilst apathy and anxiety can change people's perceptions of pain. The more non-motor symptoms a person has, the worse their pain tends to be, whilst other comorbidities can compound this or create a heightened pain appreciation.
In people with Parkinson's irrespective of disease stage, people will have an increased pain sensitivity and their nociceptive thresholds are reduced. Lewy bodies can impact parts of the brain which affect pain perception, whilst hypodopaminergic states enhance the propagation of painful stimuli all contributing to a heightened perception and sensitivity to pain. Additionally, people with Parkinson's have a lower level of analgesic neurotransmitters which compounds the problem.
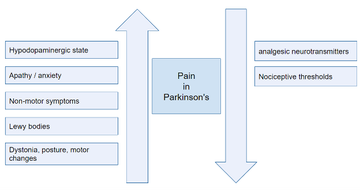
Figure 1: In summary: factors impacting pain experience in people with Parkinson's
Robin discusses the five types of pain that can be experienced by people with Parkinson's (table 1). He notes that many are under-treated and that central pain, particularly, is under-recognised and can be very distressing and significantly impactful on quality of life. He also discussed potential medications for some of these pain forms.
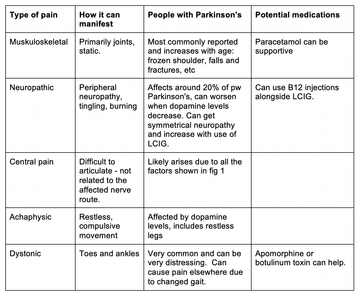
Table 1: 5 types of pain and their relation to Parkinson's
Robin issued a caution that in trying to treat some of these challenges that there can be a tendency for for prescribing to be done by both the GP and the consultant depending on whether the patient relates the pain to their Parkinson's, and people can find themselves taking multiple analgesics and dopaminergic therapies.
To avoid this, Robin advised always monitoring treatments being used and making shared decisions with the individual about whether the drug is benefiting them and meeting their current needs. Looking at smoothing out wearing off periods and looking at other non-pharmaceutical therapies to reduce pain as well. He suggested that speaking to palliative care teams can give novel ideas for pain management, and that cognitive behavioural therapy can also have a place.
He also suggested asking questions to better understand the person's pain experience, such as what the pain feels like, whether there is a pattern to it, or when it appears, whether it radiates, moves, or remains static, and so on, will all help to tailor treatment appropriately.
Robin closed the session with a case study discussion highlighting the need to get to the root cause of the pain, where possible, such as use of an SSRI where mood fluctuations impact, or dopaminergic therapies where it is a symptom of wearing off. He shared a misdiagnosis of restless leg syndrome in a patient who could not find relief from pain in his legs - when in restless legs the pain can be temporarily relieved from the movement itself. Robin shared that it became apparent the gentlemans' pain was a wearing off symptom, and that by managing his dopaminergic therapy to support slow release at bedtime, the pain was managed successfully.
'Always review - has it had a positive impact? We can't just keep escalating the dose, we need to come back and think again.'
Robin closed by highlighting the need to address sleep issues, as the association between sleep and pain is significant. Sleep deprivation can greatly increase people's pain perception, including amongst healthy individuals (Schrimpf 2015), and mood which can also impact pain perception (Woo 2010).
Questions posed by webinar attendees:
A question was posed about burning mouth syndrome. Robin responded that this syndrome is five times more common in people with Parkinson's, and may be attributable to high doses of levodopa. Reducing the levodopa burden and increasing the dopamine agonists like pramipexole or rotigotine patches can be useful if possible. Using neuropathic analgesics can be useful if the anticholinergic burden is not too high; something like pregabalin can be helpful for some people.
'On-time' dystonia particularly around abdominal muscles were asked about, and Robin noted that literature is unclear but that in practice he has also witnessed this in some patients with a sort of dystonic dyskinesia and dyspraxia breathing can also be apparent. He encouraged staying within the therapeutic window of dopaminergic therapies where possible and continuous apomorphine has also helped for some. PKGs can help with getting a good record of the individual and whether they are experiencing an 'on' dystonia.
A question around how we can differentiate Parkinson's pain from age-related pain prompted thoughts that this can be difficult, but that the fact that the patient has Parkinson's, their experience of age-related pain will be different anyway. Whilst the causes are unlikely to be disentangled, maximising dopaminergic therapies to help the individual move as well as possible will help reduce exacerbating that pain. Whilst static and joint-related pain is likely to be osteo-arthritic, the cause is less important than how to manage it going forward.
Patsy added that deep brain stimulation can be a good way of supporting people experiencing dystonia and pain early on in the condition. However, due to waiting times for this non-oral therapy, working to get oral dosing maximised in the meantime is essential.
References
Patsy Cotton:
Chaudhuri KR, Rizos A, Trenkwalder C, Rascol O, Pal S, Martino D, Carroll C, Paviour D, Falup-Pecurariu C, Kessel B, Silverdale M, Todorova A, Sauerbier A, Odin P, Antonini A, Martinez-Martin P; EUROPAR and the IPMDS Non Motor PD Study Group. King's Parkinson's disease pain scale, the first scale for pain in PD: An international validation. Mov Disord. 2015 Oct;30(12):1623-31. doi: 10.1002/mds.26270. Epub 2015 Jun 11. PMID: 26096067
Davie R. Management of Parkinson’s disease symptoms in the last days of life, 14 July 2020 Geriatric Medicine Journal. accessed https://www.gmjournal.co.uk/management-of-parkinson-s-disease-symptoms-in-the-last-days-of-life-a-review-and-guide
Higginson IJ, Gao W, Saleem TZ, et al. Symptoms and quality of life in late stage Parkinson syndromes: a longitudinal community study of predictive factors. PLoS One. 2012;7(11):e46327. doi:10.1371/journal.pone.0046327
Robin Fackrell:
Tai YC, Lin CH. An overview of pain in Parkinson's disease. Clin Park Relat Disord. 2019;2:1-8. Published 2019 Nov 28. doi:10.1016/j.prdoa.2019.11.004
Martinez-Martin P, Falup Pecurariu C, Odin P, van Hilten JJ, Antonini A, Rojo-Abuin JM, Borges V, Trenkwalder C, Aarsland D, Brooks DJ, Ray Chaudhuri K (2012) Gender-related differences in the burden of non-motor symptoms in Parkinson’s disease. J Neurol 259, 1639–1647.
Schrimpf M, Liegl G, Boeckle M, Leitner A, Geisler P, Pieh C. The effect of sleep deprivation on pain perception in healthy subjects: a meta-analysis. Sleep Med. 2015 Nov;16(11):1313-1320. doi: 10.1016/j.sleep.2015.07.022. Epub 2015 Aug 20. PMID: 26498229.
Woo AK. Depression and Anxiety in Pain. Rev Pain. 2010;4(1):8-12. doi:10.1177/204946371000400103
Our sponsor

'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.

