Before you watch this webinar
Enhancing your learning experience begins with understanding you better. Collecting data enables us to tailor our educational content specifically for our audience. Discover more about how we handle your information in our Privacy Policy.
Event
Principles of Parkinson's Neuro Examination – in person and virtually
Our sponsor

Join Dr Gemma Cummins and Patsy Cotton to discuss the principles behind Neuro examination in Parkinson's both in-person and virtually. How do they differ, what needs to be in place in order to allow optimum outcomes.
- Attendees will learn about the elements that make a good Neuro Examination and how to use those in person and virtually
- Attendees will understand the assessment that takes place prioritising patients for in person verses virtual clinics, taking into account patient preference
- Experts will share the importance of and give advice on how best to record outcome of Examination including info in GP letter that is sent to the patient
CPD accreditation
This webinar has been approved by the Federation of the Royal Colleges of Physicians of the United Kingdom for 1 category 1 (external) CPD credit(s). Please note that CPD approval does not include satellite symposia sessions. To claim the credit please email events@neurologyacademy.org.
Presentation slides – Patsy Cotton
Summary
Profile Pharma kindly sponsored the webinar on the 'Principles of Parkinson's Neuro Examination – in person and virtually' which was hosted by Daiga Heisters, attended by over 120 delegates, and featured presentations from consultant neurologist Dr Gemma Cummins and advanced Parkinson's specialist nurse Patsy Cotton.
Gemma kicked off the session by detailing the principles of a Parkinson's neurological examination and highlighting some of the red flags, before noting some of the elements specific to a virtual examination.
Gemma explained that diagnosis criteria requires both bradykinesia and at least one of the following: muscular rigidity, a 4-6 hz resting tremor, or postural instability (although this is not a feature of early Parkinson's). She then detailed all of the exclusion criteria (fig 1).
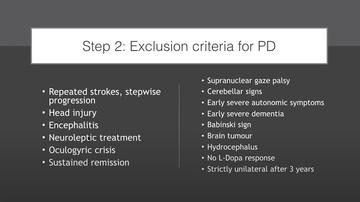
Figure 1: Gemma's slide detailing exclusion criteria for idiopathic Parkinson's disease
She talks through bradykinesia, tremor and posture looking at the ways that it can present, the different scenarios where it may be more apparent, and the different movements or activities that a patient can do during an assessment to increase likelihood of noticing this.
Gemma also outlines some differential diagnoses and the different ways that each of these areas is likely to present. She presented a case study to help demonstrate assessment and differential diagnoses.
She talks about the observations which can indicate different conditions outside of an official assessment, such as watching someone walk from the waiting room to the consulting room and noting the speed, balance and style of the gait.
She also discusses various other elements to assess either formally or in observation, including speech elements, facial clues, positive applause testing, eye movement, and even hand temperature, and the assistance each clue could give to a positive diagnosis of Parkinson's, progressive supranuclear palsy (PSP), multiple system atrophy (MSA), corticobasal disorder (CBD) or another Parkinsonian condition.
Gemma gave a case study of a young woman at 28 with young onset Parkinson's who had symptoms from age 14, and noted some of the challenges to diagnosis in young onset, the possible referrals that will be made, or the likelihood of discerning non-motor symptoms such as anxiety and depression before physical difficulties that are more commonly noted in older people.
Finally, Gemma looked at the potential to make an accurate diagnosis of Parkinson's remotely, highlighting that the majority of a good diagnosis is in the history-taking and observation, both of which can be done remotely. She then gave tips to getting a good remotely video consultation, noted some of the different assessments that can be done remotely including the MoCA, suggested physical tests that can be done in the home, and advised that the main barrier to a 'good' consultation is technology.
Parkinson's nurse specialist Patsy Cotton then discussed Patient Initiated Follow-Up (PIFU) and began her talk by posing the question: are we encouraging people with Parkinson's to self-manage? She examined this in the context of people with Parkinson's and their personal experiences of consultations, the challenges of remote consulting, and the need to empower people to manage their own health.
Patsy outlined her own experiences of managing a new caseload of 400 people with Parkinson's with one expert colleague, using a PIFU system providing a thorough discussion of the patient pathway she used (outlined in fig 2 and 3).
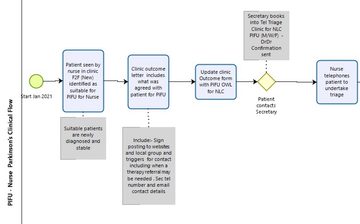
Figure 2: Patsy Cotton presents her service's PIFU flowchart - initial appointment
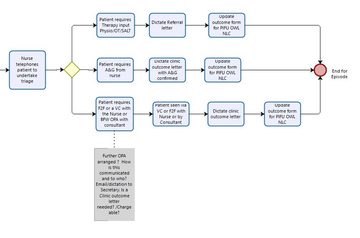
Figure 3: Patsy Cotton presents her service's PIFU flowchart - follow-up appointment
Some of the core challenges that Patsy outlined included people being lost to follow-up, thinking that one-size might fit all - when it does not - and losing sight of clinical outcomes.
She was clear that we must make every clinical contact count with patient safety first and foremost.
Gemma and Patsy then responded to a range of questions from delegates in the webinar audience, including the potential merits and challenges of making a diagnosis over a telephone consultation where an individual has no access to a video call, changing a diagnosis after a medication has already been begun, and use of the remote MoCA.
Our sponsor

'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.

