Development of the Optimal Online Guideline and Calculator for Parkinson’s Medication in Inpatients
The guideline and calculator has been developed and can be accessed here: www.parkinsonscalculator.com
Medicines management is crucial in the care of the patient with Parkinson’s when they are admitted to hospital either electively or in an emergency.
Missed doses can impair patients’ swallow, increase their risk of aspiration, render them immobile and prone to falls and fractures and – at worst – lead to Neuroleptic Malignant-Like Syndrome, which can result in coma and death. Particular problems arise if a patient is placed nil-by-mouth, or is unable to take their usual Parkinson’s medication due to their concurrent illness.
Guidelines for inpatient Parkinson’s medication management painstakingly developed by various acute Trusts around the country are not available or collated nationally. Furthermore, existing drug conversion tables and algorithms for patients who cannot take their usual Parkinson’s medications are complex, cumbersome and carry a high risk of calculation errors. In this digital age, surely there is a better way?
The OPTIMAL online guideline and drug conversion calculator were originally developed at University Hospital Southampton and Poole Hospital, to help nonspecialist clinical staff to better manage patients with Parkinson’s when admitted, better plan for elective admissions and direct staff to sources of specialist support. With the support of Parkinson’s UK and the British Geriatrics Society (BGS) Movement Disorders Group, we hope soon to make this resource available nationally and freely, and all at the click of a mouse.
Background
The scenarios are all too familiar: the septic and delirious patient with Parkinson’s admitted to the acute medical unit on a Friday evening and unable to swallow their Parkinson’s medication; or the perioperative Parkinson’s patient who is nil-by-mouth or unable to absorb their medication due to gastrointestinal issues. We as Parkinson’s specialists are often consulted some time down the line, usually after the patient has developed complications as a result of missing their medication. Worse still, signs of dopamine withdrawal can go unrecognised or be misinterpreted as deterioration in the patient’s intercurrent illness. It was just such a scenario that prompted the development of the OPTIMAL online guideline at University Hospital Southampton. to say that guidance is not already available to assist in these situations. Many trusts have developed their own clinical guidelines for medicines management in Parkinson’s, displayed on posters or intranet sites. It is the accessibility of this advice that is the problem. How many of our surgical or junior colleagues know where to find guidance on Parkinson’s medication? And if a hospital does not have its own guideline, what then?
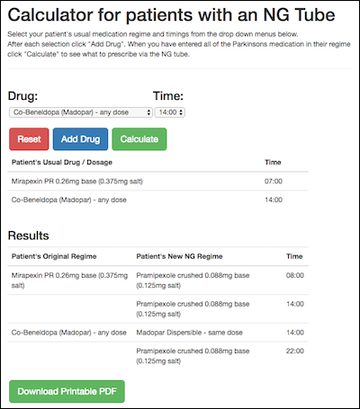
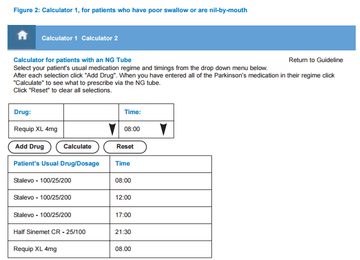
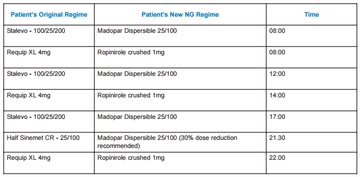
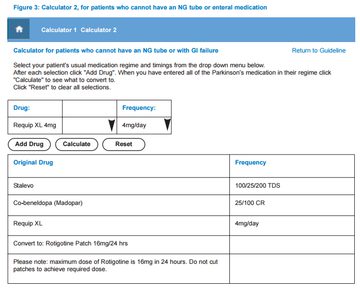
It doesn’t stop there. Once a guideline has been located, using the accompanying tables or algorithms to convert patients’ usual medication to a dispersible preparation via a nasogastric (NG) tube or to a parenteral alternative can be arithmetically challenging even for Parkinson’s specialists, and vulnerable to error. A nationally available guideline with an electronic drug conversion calculator has the potential to address these clinical issues, and provide an educational resource for Parkinson’s specialists and nonspecialists alike.
THE OPTIMAL GUIDELINE
The basic guideline is shown in Figure 1. The user is led through a 7-point flow diagram reminding them of the importance of an accurate and specific drug history and prescription with attention to the patient’s usual timings, drugs to avoid, and links to drug conversion calculators for patients who are nil-by-mouth or cannot absorb enteral medication. Finally there are prompts to resume the patient’s usual Parkinson’s medication regimen as soon as possible, and to contact a Parkinson’s specialist at the earliest opportunity.
Step 7 could be adapted by individual hospitals to include names and contact numbers for local PD specialists.
The Calculators
Worked examples are shown below for a patient who usually takes Stalevo 100/25/200 three times daily, Requip XL 4mg once daily and Half-Sinemet CR nocté. Figure 2 (below) demonstrates use of Calculator 1 to convert the patient to preparations that can be passed down an NG tube if their swallow is poor or they are nil-by-mouth, with attention to timings.
In Figure 3, below, a similar regimen (this time with Madopar 25/100 CR rather than Half Sinemet CR) is converted using Calculator 2 to an equivalent dose of transdermal rotigotine for patients with enteral failure or in whom NG intubation is not appropriate or technically feasible.
Challenges and Next Steps
OPTIMAL is currently being piloted locally and audits of Parkinson’s medication errors and complications before and after its introduction being undertaken. Getting to this stage has been no mean feat: reaching agreement on the guideline and drug conversions amongst local Parkinson’s steering groups, developing the online software and gaining local Drugs and Therapeutics Committee approval to list but a few of the challenges. It is for this reason that we are keen to save others from duplicating this work and are liaising with Parkinson’s UK to make the resource available nationally via their website, as part of the UK Parkinson’s Excellence Network. Both the BGS Movement Disorders Group and the Association of British Neurologists have expressed their support for this endeavour.
Fine-tuning of the resource is ongoing, and it is hoped that a mobile app could also be developed in the future. Additional functionality including the ability to obtain printouts, the potential to link in with online prescribing software and its educational role are also being explored.
So watch this space. The future’s bright. The future’s OPTIMAL.
Dr Naomi Fox, Consultant Geriatrician
Poole Hospital NHS Foundation Trust
Update: the OPTIMAL online calculator is now available here: www.parkinsonscalculator.com
References
- MacMahon, M. and MacMahon, D. (2012) ‘Management of Parkinson’s disease in the acute hospital environment’, Journal of the Royal College of Physicians of Edinburgh 42: 157-162.
- NICE (2006) Parkinson’s disease. Diagnosis and management in primary and secondary care. London.
Acknowledgements
- Dr Gayle Strike, Consultant Geriatrician, University Hospital Southampton NHS Foundation Trust
- Ben Fox, IT Developer
- James Allen, Senior Pharmacist, University Hospital Southampton NHS Foundation Trust
- Suma Surendranath, Parkinson’s UK
More Parkinson's Academy Medication Projects
'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.