Implementing an improved referral pathway to enhance specialist inpatient review of patients with a diagnosis of Parkinson’s disease at the Bristol Royal Infirmary
Poster
Introduction
Parkinson’s disease (PD) is a chronic, progressive, neurodegenerative disorder, requiring specialist input to optimise its management. COVID-19 has further impacted on the care of these patients as clinic appointments were cancelled. The referral process to the Parkinson’s team was previously unclear, with some junior doctors unaware the service existed.
This project therefore aimed to improve the referral process for inpatients with PD, providing opportunistic specialist reviews including medication optimisation, management of associated symptoms and ongoing community review.
Methods
A new online referral pathway via CareFlow was created in February 2021 and promoted to medical staff via email, poster displays and demonstrations on the use of CareFlow. There were also dedicated teaching sessions for the ward staff on the inpatient management of patients with PD. All known patients with PD within the trust via CareFlow system were “pinned” to the “BRI Parkinson’s & Movement disorders team” and then a “tag” labelled “Parkinson’s disease” was added , allowing the movement disorders team to be automatically informed of inpatient admissions.
In addition ward teams could raise a referral via CareFlow requesting a review of a patient on their wards, including those with a suspected new movement disorder. Once seen the movement disorder team could edit the referral adding the outcome and raise a task e.g. for a re-review (with a date), communication (letter to the GP). Once a referral was complete it would be marked as “cancelled.” The referral information including reason for referral, speciality referred from and who had seen the patient allowed for simple retrospective auditing of the use of the system.

Results
Awareness amongst staff
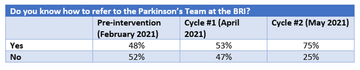
Post-intervention survey results showed a small increase in awareness of the Parkinson’s referral pathway after email promotion with a further increase after displaying posters in prominent locations and delivering demonstrations (from 48%, to 53%, to 75%).
During cycle 2 of data collection, medical staff were also asked why an inpatient Parkinson’s service is important. Common themes included recognising the need for specialist medical input, the importance of regular review of medications and associated symptoms (noting the lack of this during the COVID-19 pandemic) and the multi-disciplinary approach to care.
Referrals
- Referrals were reviewed over a 6 months period from the end of February 2021 – end of August 2021.
- A total of 112 inpatient PD reviews occurred.
- Average of 5 patients reviewed a week.
- Average of 19 patients reviewed per month.
- Only 2/3 of the patients with a prior diagnosis of a PD were known to the BRI movement disorders team with others known to neighbouring trusts inc North Bristol, Weston General Hospital and Taunton.
- Of the referrals for suspected PD: 20% had probable IPD, 47% had a probable parkinsonism (inc. drug induced and vascular), 6% had probable LBD.
- 42% of patients received a PD medication change during their admission this included those who needed to receive the medications via other routes e.g. NG, patch and went back to their usual regime at discharge.
- Only 19% of patients with PD were care for on a care of the elderly (COTE) wards.
- 18.3% of patient died that admission or in the 30 days post discharge.
- A letter informing the community teams inc PD practitioners and GP of an inpatient PD review was sent for 2/3 of patients.
- 44% of referrals were seen by a registrar, 56% by a consultant. All SpR reviews were discussed with a consultant. But job planning in the future some of these patients (on discussion and support of the movement disorders consultant) could have been reviewed by other members of a MDT:
- Of the referrals 56% were deemed appropriate to have been seen by a PD practictioner.
- 97% of patients were deemed to be appropriate to have been reviewed by a clinical fellow with experience in movement disorders.
- 24% were highlighted to be appropriate to have been reviewed by a pharmacist with experience in movement disorders.
Conclusions
The introduction of an online referral pathway for inpatient Parkinson’s reviews has led to increased awareness of the service among medical staff at the BRI.
Physician associates were also included in teaching sessions due to their continued presence on medical wards, encouraging retention of this knowledge.
Junior doctors recognise the importance of this service, referring patients for the specialist input integral to managing a complex condition.
Accurate recording on the number of inpatient movement disorder reviews will help with job planning in the future. Acknowledging that there is a paucity of senior medical doctors with an interest in movement disorders, there is scope to look at the role of MDT members with a specialist interest in PD supporting the service.
With unprecedented bed pressures the majority of inpatients with PD are not being cared for on COTE wards making easier access to referrals to specialists even more important.
18.3% of patients died during the admission or in the 30 days after admission showing it is never too early to consider ACP with this patient cohort.
From a staff development perspective when clinics are cancelled due to a pandemic. Supervised inpatient PD reviews are a valuable learning opportunity.
More Parkinson's Academy Care pathways Projects
'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.