Is there a need to improve timings of doctor and Parkinson’s disease nurse specialist appointments to improve patient care?
Poster
Background
In March 2021 I took over a Parkinson’s disease clinic which runs out of a community hospital in Romsey. The service is run by Southern Health NHS Foundation Trust. The patients who attend the Romsey clinic (RC) are seen either by a consultant or specialist registrar. Attached to the clinic is a Parkinson’s disease nurse specialist (PDNS) who works for Hampshire Hospitals NHS Foundation Trust. The PDNS covers multiple areas of which the RC is just one.
There is a perception that there is often unintentional overlap of appointments between the RC and PDNS which is an ineffective use of clinical time and does not provide best patient care. This overlap of appointments is felt to be due to the fact that the RC and PDNS appointments are run by two separate trusts, with two different administration teams.
Aim
To establish if there is a significant burden of appointment overlap between the consultant led RC and the PDNS appointments and if so, to find a clerical solution to rectify this.
Method
The RC has a legacy database of the patients that are thought to be under the care of the clinic of which there are 74 patients. I reviewed the clinic letters of these 74 patients over three years (from 19/8/2018 to 19/8/2021) and collected the following data:
Age
Year of diagnosis
Dates of all the clinic appointments within that time period
Whether the appointment was with the RC or the PDNS
Using the above data, the gap between appointments (in weeks) could be established. It could also be established which patients were being seen by both the RC and the PDNS. There are some patients at the clinic who prefer not to engage with the PDNS and are therefore only under the care of the RC. There are also some patients who are too frail to come to clinic and are seen only by the PDNS in the community. Only patients who had a mix of appointments between the PDNS and the RC were included in the analysis (“Group D+N” i.e. Group Doctor+Nurse).
Results
Number of patients on the database = 74
1 Discharged to GP
5 Lost to follow-up / no longer live ‘in area’
Number of patients under active follow-up = 68
Number of patient’s being seen by both RC and PDNS to be included in the analysis (Group D+N) = 45
Group D+N (Patients receiving both PDNS appointments and RC appointments)
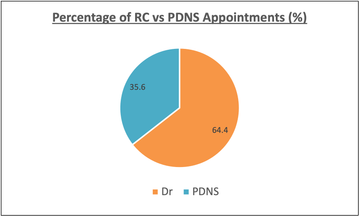
Total number of appointments between 19/08/2018 and 19/08/2021 = 405 (261 with RC, 144 with PDNS)
Analysis of Gaps Between Appointments
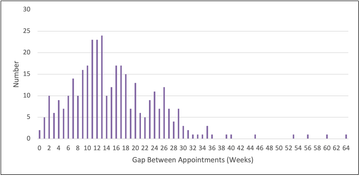
The median gap between patient’s appointments was 13 weeks (range 0 weeks to 64 weeks)
Analysis of Appointments with a Gap ≤4 weeks (“Close Follow-up” Appointments)
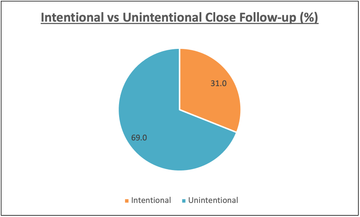
Number of times gaps between appointments occurred ≤4 weeks = 29.
Analysis of the letters either side of these gaps showed that the close follow-up was only intentional in 9 of these cases (31%). 20 being unintentional.
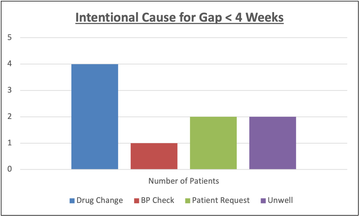
The reasons given for an intentionally close follow-up were as follows:
However, the total number of ‘gaps’ between all the appointments of patients in Group D&N = 360. 20 ‘unintentional’ close follow-ups only represents 5.55% of all the gaps between all appointments.
All of the unintentional close follow-ups occurred between appointments between the RC and PDNS (as opposed to between two RC appointments or between two PDNS appointments).
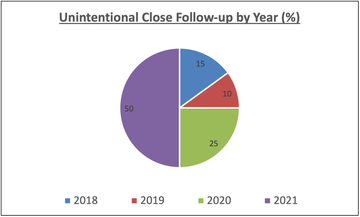
Further analysis of those patients who had an unintentionally close follow-up showed that 75% of these occurred during the pandemic (2020 – 2021).
Discussion
It was an informative process to manually go through all the patients on the legacy database as I was able to discover that 6 were no longer under active follow-up. Indeed, I was able to investigate some that had seemingly been ‘lost to follow-up’. In all cases they had moved out of area.
There is limited official guidance on how frequently patients with Parkinson’s disease should be followed up. NICE guidance suggests that they should be reviewed “every 6 to 12 months”. The median age of this cohort of patients was 80 years old. The median number of years since diagnosis was 9 years. This represents a relatively older and more advanced group of patients that you might expect to have more frequent follow-up. The median follow-up gap in this cohort was 13 weeks (2.99 months). Despite this, follow-up in under 4 weeks would be unusual.
Analysis of the patients who were followed-up in less than 4 weeks showed that 69% of these received unintentionally close follow-up. This is due to, as mentioned in the introduction, the appointments for the RC and the PDNS appointments being managed through two different trusts. However, as mentioned in the results, these unintentionally closely followed-up appointments only count for 5.55% of the total number of appointments over the three years. Overhaul of secretarial systems across two trusts is unlikely to resolve the issue and is would not be a good use of resource. A better approach is likely to be to empower the patients, and their carers, to be aware of when follow-up is planned (verbally and in writing in their letters) and ask them to challenge the booking teams if appointments come too close together.
Furthermore, the results showed that 75% of the unintentionally close follow-up appointments occurred in 2020/2021. That is to say, during the pandemic. During this time the administration departments across both trusts were disrupted. In addition, patients may well have altered the scheduling of their appointments in an attempt to avoid direct hospital attendance (which would not necessarily be recorded in clinical letters).
Conclusions
- Appointment overlap is less frequently an issue than anticipated. Empowering patients and their carers to challenge when they receive appointments close together may be an effective way to approach this issue when it does occur. In order to do this, intended follow-up should be routinely documented in all letters.
- Appointment overlap occurred more frequently during the pandemic. The reasons for this are not clear but hopefully as the pandemic disruption improves this will occur less often.
More Parkinson's Academy Policy & guidance Projects

'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.