Tools for change: creating practical ways to improve quality, care and support
KnowledgeThere are some incredible individuals whose passion for people, and belief that change starts with them, have revolutionised the way care looks on a daily basis. We have been interviewing some of them for our Star Showcase and hope you have been enjoying hearing about their journeys and their practices as Parkinson’s specialists.
Sometimes, the difference between basic and brilliant care is a practitioner who listens thoroughly, communicates effectively and responds efficiently. Sometimes it’s a can-do attitude and a refusal to compromise. Sometimes it’s a brilliant team rapport, or positive lines of communication across departments.
And sometimes, it’s a tool.
That tool can be a complicated little gadget with heaps of functions, or it can be a piece of paper with the right questions on it, but a tool can sometimes be the difference between sub-optimal services and truly outstanding care.
Some of our Stars have created their own tools as part of the change they are affecting in Parkinson’s care and support in their areas. We want to highlight those tools, and perhaps a few others besides, that might help you to switch up the services you are part of. So here they are, the tools for change. Some simple ways that Parkinson’s care can ‘up its game’.
Use existing free gadgets
Supporting a Parkinson’s patient on a hospital ward can be tricky - medication must be given at exactly the right time, in the right quantity, and managing this alongside lots of other patients can be a challenge. If that patient becomes nil by mouth, it gets even harder. Working out the right quantities of the equivalent medicine to be given via a naso-gastric or ‘PEG’ feeding tube can be rather daunting.
This medication calculator was developed by Dr James Fisher and is accessed online. With quick and easy drop-down boxes, the user inputs the patient’s usual medication type, quantity and frequency, and the tool calculates the equivalent dose to be given via PEG. It has over 10,000 visits to the site to date and is a simple and very effective tool to make sure people with Parkinson’s get the right medication at the right time, all the time.

Medication calculator developed by Dr James Fisher
Get everyone on the same page
Sometimes the simplest tools are the most effective. Specialist nurse Louise Ebenezer developed a simple form to use in the hospital she works in so that patients with Parkinson’s are flagged up to her before they receive any treatment. A similar system has been set up by Dr Richard Genever, with the pre-assessments clinic flagging Parkinson’s patients who are being treated under other departments or specialisms.
For both, they feel they can plan in advance for any requirements like nil by mouth or specific rehabilitation, providing support to their patients, and also to the professionals caring for them. With one piece of paper, everyone gets on the same page.
Draw on existing service models
Phrases like ‘don’t throw the baby out with the bathwater’ and ‘don’t reinvent the wheel’ are often used around service improvement or redesign, and whilst they are fair, they can hold back change, or produce services with extra bits tacked on, making them clunky or tricky to navigate.
However, trying to create a really positive service doesn’t have to mean designing it from scratch - there are some excellent models of care that we can draw on, learn from, or simply replicate. They often have already looked at how they support government strategy, better use resources, meet policy guidelines, and overcome hurdles so that you can start from the other side of them. A set of tools just like this, from service designs to business case templates, are part of the MasterClasses and are shared with all attendees to support them back in their practice.
Whether drawing on templates like this, following renown models of care like the Parkinson’sNet model as Neil Archibald did, or using an existing service like the Parkinson’s Advanced Symptoms Unit as a blueprint, high quality services are tools in themselves to be used as learning or to create frameworks for replication.

Parkinson’sNet model
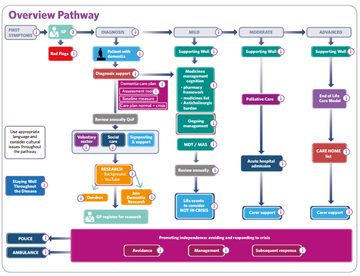
Use an existing interactive care pathway
Interactive care pathways, or ICPs, have been developed in a number of sites in various guises and can be a brilliant tool to draw on or replicate. This can be done for whole services, or individual specialist elements of care such as managing a relapse in MS, supporting a positive end of life, or treating a particular symptom of Parkinson’s like dementia.
The Dementia ICP, developed by the Dementia Academy, is a free online resource, whilst other localities have their ICPs available to view, or their learning shared online.
Dementia interactive care pathway toolkit
Teaching your peers
Whilst teaching may not seem like a standard tool, it is no doubt a brilliant way to improve the quality of care delivered across a whole healthcare locality. By upskilling peers across other departments whether informally or through planned training, someone with Parkinson’s can be treated holistically and with confidence no matter where they come into the service. Sarah Marrinan found that offering training sessions has resulted in better care for individuals and more confident professionals. By building those relationships, non-specialist professionals are more likely to seek support in complex situations too.
Decipher your data
Understanding data, specifically quantitative data like Hospital Episodic Statistics (HES), can be really valuable tool to unravelling what is happening in your service or your overall locality. Dr Andrea Lindahl and colleague Dr Lucy Strens have helpfully documented their experiences with data, including HES, in building a Parkinson’s service - and you can learn more about that service in Andrea’s story.
‘The more I learn about Parkinson’s, the more I realise how much more there is to learn and understand’ – Louise Ebenezer
Go on a MasterClass
Education itself is a tool. A number of our Stars have noted that we never stop learning, and so never stop improving our practice, and our Founding Faculty all link the movement for education with the revolution in care over the past two decades. Increasing your own knowledge, understanding and confidence could be the tool you need to kickstart change in your locality. Geriatrician Dr Ed Richfield’s focus on rethinking palliative care for Parkinson’s spurred him to create the Palliative Care MasterClass with the Neurology Academy, knowing what a powerful tool knowledge can be in implementing change.
Related articles
'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 22 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. Led by co-founder and educational director Dr Peter Fletcher, the Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.


