Impulsive and Compulsive Behaviours
Impulsive and compulsive behaviours: How well is advice regarding these side effects recorded in the notes, both at initiation of treatments and on follow up?
Background
In recent years Impulse Control Disorder (ICD) has been more widely recognised as a possible side effect of some drugs used for the management of Parkinson’s disease, particularly use of dopamine agonists. The Parkinson’s UK website quotes the incidence as being up to 17%. The website goes on to say that although there are identified risk factors associated with the likelihood of a patient developing ICD, and that 82% of consultants in a survey had seen someone with ICD, only 48% of consultants routinely screen.
Reports on the Parkinson’s UK website and from anecdotal evidence illustrate how these symptoms can be devastating to patients and their families. Whilst carrying out this project a patient, known to our clinic and taking Ropinerole, was admitted to the ward and while on the ward the nursing staff highlighted his inappropriate behaviour towards them. This initiated conversations with their spouse, who was distressed as she recounted how difficult it had been for her at home and she hadn’t told anyone. This highlights, the sensitive nature of some of these behaviours and the need for us as clinicians to create the environment in the clinic for patients and their spouses to be open and honest with us.
This audit was designed to look at how well advice regarding these symptoms was recorded in the notes both when treatment was initiated and at follow-up visits.
Method
This was a retrospective notes study. From the 220 sets of notes of patients attending the Parkinson’s clinic at Royal Victoria Hospital, Dundee, 34 were identified as being currently on Ropinerole, Rotigotine or Pramipexole. I went through the notes taking information from the GP letters and the UPDRS score sheet which is completed for each of our patients at their annual review.
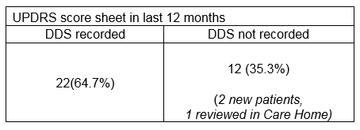
I looked specifically for mention of ICD at initiation of treatment, and the first follow up appointment and then at their last review appointment. I then reviewed all the UPDRS sheets to check for completion of the Dopamine Dysregulation Syndrome box.
Results
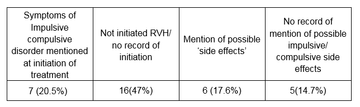
At initiation
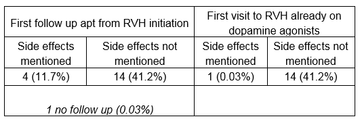
First follow-up or review appointment
Last review appointment
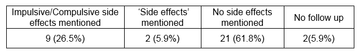
On looking through the GP notes advice to the patient was often recorded as ‘side effects’ and therefore not always obvious whether this meant impulsive or compulsive behaviours had specifically been spoken about. The results are therefore recorded separately as when ICD was specifically mentioned or when ‘side effects’ were noted.
47% of the patients identified had not had their treatment initiated at RVH, therefore I looked to see if ICD had been mentioned in the letters at their first visit to RVH.
Discussion
From the results shown it would suggest that recording of whether these specific side effects have been discussed with the patient is not particularly well done. There are limitations, the main one being that the side effects may well have been discussed but this discussion not recorded in the GP letter. From my background as a GP I would suggest, that the GP may well have known the patient and their family for a considerable length of time and it might be in the community that the patient is more comfortable to speak about these issues and so highlighting it to the GP is of specific importance.
As a result of this audit I met with the two consultants who run the Parkinson’s clinic to look at how we could take this forward. I showed them the ‘Impulsive and compulsive behaviour in Parkinson’s monitoring and information tool’ produced by Parkinson’s UK. Following discussion we agreed that whereas the tool is excellent, and we would look at incorporating this into practice, this is just one small part of all that needs to be discussed and recorded in a Parkinson’s consultation, so is it right to look at one part in isolation? We agreed that the way forward would be to develop a Parkinson’s clinic review sheet, which ideally could also become a template for the GP letter. We are still in the process of developing this.
References & Acknowledgements
With thanks to:
Gillian Strachan, medical secretary MFE, RVH
Dr Derek Sutherland Associate Specialist MFE
Dr Deepa Sumakadas Consultant MFE
Written by:
Dr Carolyn Tipton
Specialty Doctor, Medicine for the Elderly
Royal Victoria Hospital
Dundee
More Parkinson's Academy Cognition Projects
'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.