Parkinson’s pathway, The first 24 hours in Hospital
Goal is:
To identify problems in the management of Parkinson’s medications in patients acutely admitted to Weston general Hospital.
We identified the gaps in awareness of available PD service and identified the need for a local guidance and a pathway for acutely admitted PD patients.
Problems
We identified that errors in prescription of medications are multifactorial. Lack of awareness of help available amongst junior doctors, medication availability and lack of local trust guidance are some of those factors.
Plan
Develop local guidance and a pathway for acutely admitted PD patients.
Implementing the pathway and developing a web page with all the information regarding PD in our trust.
Measure improvement in PD patient ‘s care on admission to Weston General Hospital.
A long term ambition is to develop a consortium to establish registry for Parkinson’s patients in our catchment area.
Methods
A survey of junior doctors regarding their knowledge of PD management priorities and the need for trust guidance was undertaken.
Develop pathway and local guidance and make them available on the intranet
Teaching sessions for junior doctors and other members of the MDT
Measure the effects of our interventions:
- looking at accuracy in PD prescriptions
- improved confidence in switching formulation
- Implementing the pathway and guidance for all PD patients admitted.
Pre-intervention data

The pre-intervention survey shows some gap in awareness regarding properly and timely managing patients with Parkinson’s on admission to Weston General Hospital.
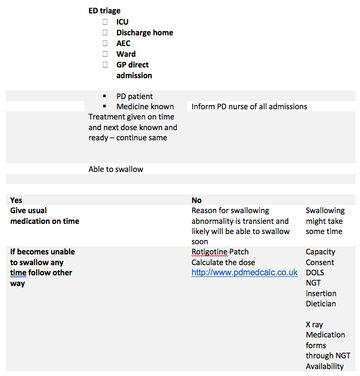
Admission
Ambulance
- Known Parkinson’s :
- YES
- NO
- NOT sure
- Other movement disorders
- Current medications : Name, dose and frequency /form
- –
- –
- –
- –
- –
- –
- Last time taken his / her medicine
- –
- –
- –
- Next DUE medicine include dose and time
- –
- –
- –
- Last time opened his / her bowels
- Is able to swallow his / her medicine
- Yes
- No
- If not sure of medicine and last dose and due dose GIVE a stat dose of :
- dispersible tablets ( 125 mg co-beneldopa) if able to swallow or on NGT
- or prescribe a Rotigotine patch 2mg if not able to swallow / not on NGT or awaiting NGT
TRAIGE
- Consider the time patient has to wait before sorting out the reason for admission and stabilizing his condition if unstable
- Giving the due dose of Parkinson’s medicine is a clinical priority for all triage pathways and must be confirmed as given during handover. Tick if Given
- Those patients awaiting to be seen or awaiting transport home must receive their prescribed Parkinson’s medicine on time without any delay
- If medicine is not given for any reason, must escalate to senior staff member
- If unable to swallow give patch, consider NGT insertion, refer to SALT team
- Consider the time needed to insert NGT and confirm its position. If delay is expected then use a Rotigotine patch until safe to use NGT
- If NGT inserted refer dietician for enteral feeding
- Refer all cases to PDNS Sarah Barber bleep number 329
- Refer all patients who cannot swallow to SALT for assessment
- Consider PR and abdominal X-ray if indicated by abdominal examination
- Lying and standing blood pressure in all
- Medications available on ED / MAU / Kewstoke ward Stock
- Medicine is always available through on call pharmacist and onsite manager
- Regardless of the cause for admission PD GET IT on TIME is a clinical priority even if reason for admission is for social reasons and nil acute
- Any patient with PD referred to Palliative care or considered for palliative care must be reviewed by PDNS / PD team / consultant with PD experience
- Monitor for
- Constipation
- Retention of urine
- Hallucinations
- Sleep
Medication Management
- Avoid stopping , omitting ,missing or prescribe differently
- Avoid metocloprimide, haloperidol, prochlorperazine, and cyclizine
- Avoid Abrupt cessation of antiparkinsonian medications which may lead to the development of neuroleptic malignant syndrome (NMS), or a dopamine agonist withdrawal syndrome (DAWS).
More Parkinson's Academy Care pathways Projects
'The things you can't get from the books'
Parkinson's Academy, our original and longest running Academy, houses 23 years of inspirational projects, resources, and evidence for improving outcomes for people with Parkinson's. The Academy has a truly collegiate feel and prides itself on delivering 'the things you can't get from books' - a practical learning model which inspires all Neurology Academy courses.